Background: Electrical storm (ES) is associated with a high mortality and further leads to recurrent hospitalization due to worsening of heart failure or repeat ICD therapy deliveries. Catheter ablation of ventricular tachycardia (VT) has proven to be successful in reducing ventricular arrhythmia recurrences. The current ESC guidelines give a class Ib recommendation for timely VT ablation in ES. Nevertheless, the exact timing of VT ablation needs to be further elucidated, especially since structural prerequisites for centers serving with prompt catheteter ablation in the setting of ES are challenging.
Aim: The purpose of this retrospective single-center study was to analyze treatment success using standardized management in patients with electrical storm. Study endpoints were acute success of treatment, patient mortality, recurrent hospitalization and VT recurrence.
Methods: Data from consecutive patients who suffered one or more ES from 2016 to 2021 were analyzed. Patients were divided into 3 groups based on the treatment they received: Group 1: VT ablation within <10 days after ES onset, group 2: VT ablation within >10 days after ES onset, Group 3: conservative therapy. Until 2018 ES treatment mainly consisted of conservative therapy. After a change of the institutional protocol the standard treatment was changed to catheter ablation. The timepoint of ablation was determined on individual decision for each patient, reflecting the clinical situation as well as logistic reasons. Follow-up (FU) was performed by telephone, telemedicine monitoring and assessment of the hospital information system. Primary endpoint was all-cause death, LVAD (left ventricular assist device) implantation and heart transplantation (HTX) within 12 months after treatment. Secondary endpoints were recurrent VT with ICD shock, recurrent ES and hospitalization.
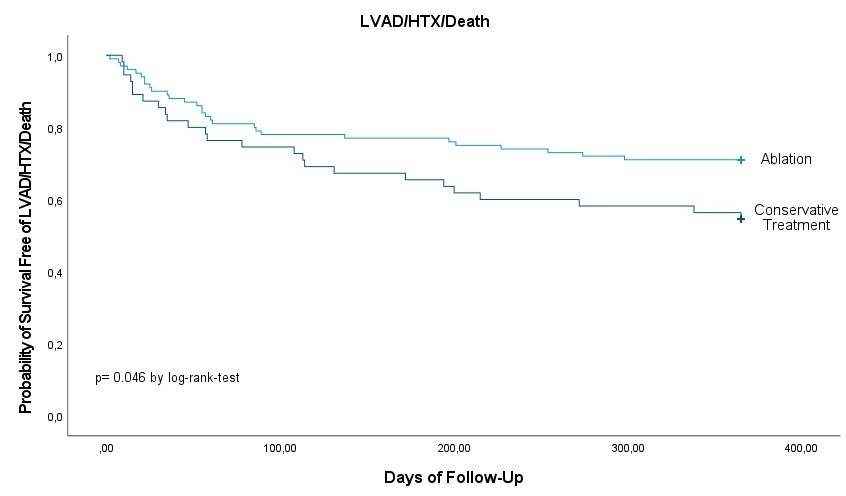
Results: A total of 155 patients were analysed (Group 1, n=50; Group 2, n=50; Group 3, n=55). There were no significant differences in the baseline characteristics, except of the higher use of class I and III antiarrhythmic drugs previous to ES in group 1 and 2 (27 and 27 patients, 54% each) compared to 15 patients (27%) in group 3 (p=0.002) and a higher amount of patients with a history of catheter ablation in group 1 (19 patients, 38%) as compared to 12 (24%) patients in group 2 and 6 (11%) in group 3 (p=0.005). After a 1-year FU, the combined primary endpoint occurred in 13 (26%) in group 1, 16 (32%) in group 2, and 25 (45%) in group 3 (p=0.110). There was a significant reduction for catheter ablation (groups 1 and 2) with 29 patients (29%) reaching the study endpoint compared to conservative therapy (25 patients, 45%) (p=0.046 by log-rank-test). There was no significant different in analysis of secondary endpoints, including VT recurrence with ICD shocks and rehospitalization.
Conclusion: VT ablation of ES was associated with a lower risk of death, LVAD implantation and HTX within a 1-year as compared to conservative therapy.
Aim: The purpose of this retrospective single-center study was to analyze treatment success using standardized management in patients with electrical storm. Study endpoints were acute success of treatment, patient mortality, recurrent hospitalization and VT recurrence.
Methods: Data from consecutive patients who suffered one or more ES from 2016 to 2021 were analyzed. Patients were divided into 3 groups based on the treatment they received: Group 1: VT ablation within <10 days after ES onset, group 2: VT ablation within >10 days after ES onset, Group 3: conservative therapy. Until 2018 ES treatment mainly consisted of conservative therapy. After a change of the institutional protocol the standard treatment was changed to catheter ablation. The timepoint of ablation was determined on individual decision for each patient, reflecting the clinical situation as well as logistic reasons. Follow-up (FU) was performed by telephone, telemedicine monitoring and assessment of the hospital information system. Primary endpoint was all-cause death, LVAD (left ventricular assist device) implantation and heart transplantation (HTX) within 12 months after treatment. Secondary endpoints were recurrent VT with ICD shock, recurrent ES and hospitalization.
Results: A total of 155 patients were analysed (Group 1, n=50; Group 2, n=50; Group 3, n=55). There were no significant differences in the baseline characteristics, except of the higher use of class I and III antiarrhythmic drugs previous to ES in group 1 and 2 (27 and 27 patients, 54% each) compared to 15 patients (27%) in group 3 (p=0.002) and a higher amount of patients with a history of catheter ablation in group 1 (19 patients, 38%) as compared to 12 (24%) patients in group 2 and 6 (11%) in group 3 (p=0.005). After a 1-year FU, the combined primary endpoint occurred in 13 (26%) in group 1, 16 (32%) in group 2, and 25 (45%) in group 3 (p=0.110). There was a significant reduction for catheter ablation (groups 1 and 2) with 29 patients (29%) reaching the study endpoint compared to conservative therapy (25 patients, 45%) (p=0.046 by log-rank-test). There was no significant different in analysis of secondary endpoints, including VT recurrence with ICD shocks and rehospitalization.
Conclusion: VT ablation of ES was associated with a lower risk of death, LVAD implantation and HTX within a 1-year as compared to conservative therapy.
https://dgk.org/kongress_programme/jt2023/aV713.html