Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02180-w
|
|
A rare case of heart failure due to aseptic shunt between left ventricular outflow tract and left atrium after aortic valve replacement
|
|
I. von Scheidt1, G. Waidhauser1, B. Wein1, S. Elvinger1, P. Raake1, E. Harmel1
|
|
1I. Medizinische Klinik, Universitätsklinikum Augsburg, Augsburg;
|
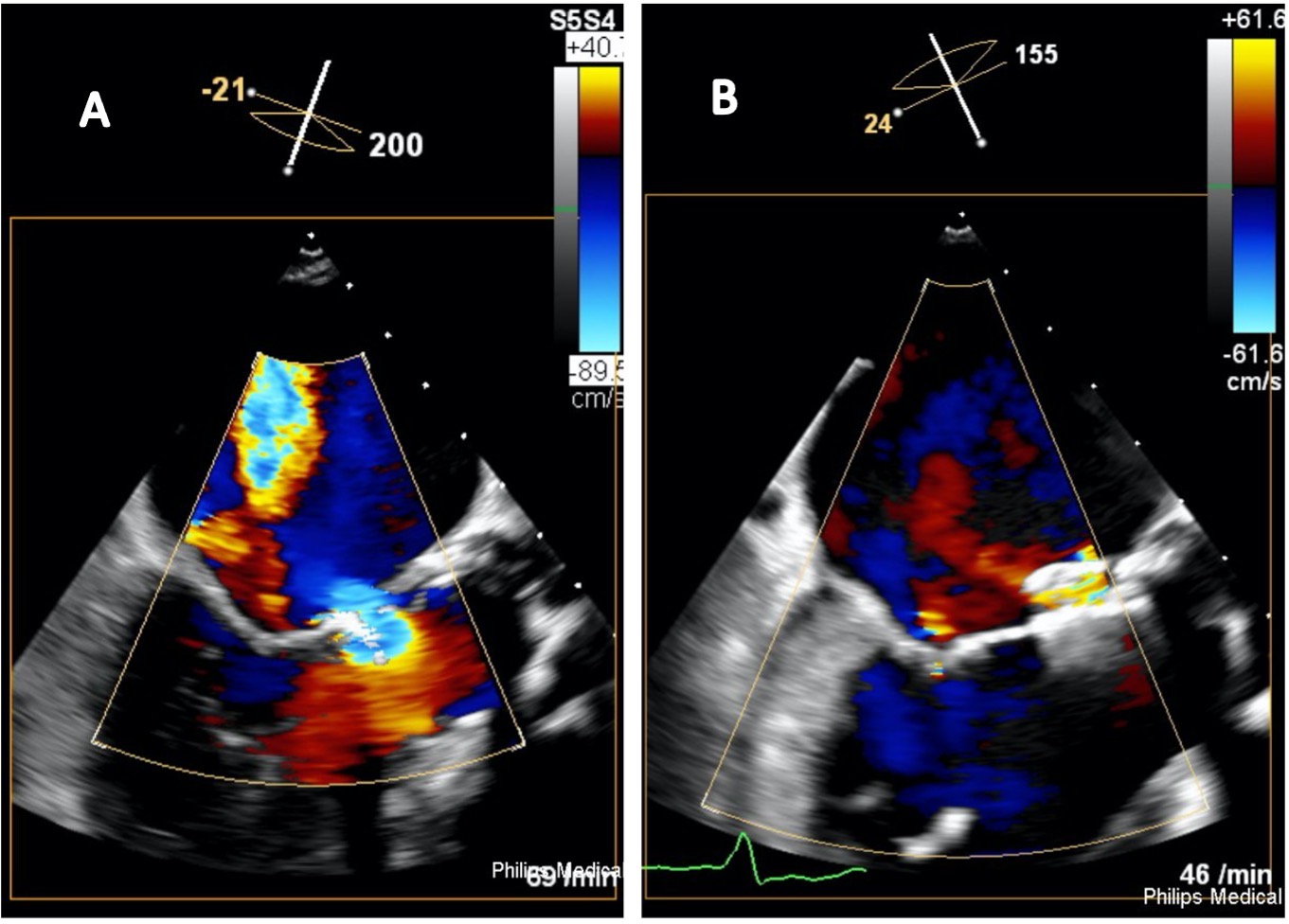
A 79-year-old male patient was admitted to hospital with progressive dyspnea in New York Heart Association (NYHA) functional class III-IV and signs of fluid overload. Electrocardiogram showed new onset atrial fibrillation and the NT-proBNP level at time of admission was elevated to 16.451 pg/ml. Since past medical history revealed a status post aortic valve replacement with a bovine biological prothesis and clinical examination found a systolic heart murmur, an early valve deterioration of the biological prothesis was assumed. Contrary to expectations, transesophageal echocardiography (TOE) showed excellent valve function of the bio prothesis and no signs of other valvular pathologies or lesions consistent with infective endocarditis. However, a subannular perforation of left ventricular outflow tract (LVOT) in the region of fibrous aortomitral continuity was detected, thus resulting in a significant LVOT to left atrial (LA) shunt (figure A) with a peak systolic LVOT-LA pressure gradient of 91 mmHg and both, severe LA and left ventricular enlargement. Right heart catheterization confirmed isolated postcapillary pulmonary hypertension with pulmonary capillary wedge pressure of 23 mmHg and elevated v-wave signal, consistent with significant LVOT-LA shunt.
Despite high doses of intravenous diuretics, recompensation was prolonged and poorly tolerated. Therefore, heart team decision was in favor of catheter-based shunt closure.
At first, a transaortic approach for shunt passage was chosen using an internal mammary artery guiding catheter. Since no stable catheter position in the LVOT was achievable, the procedure was changed to a transseptal approach. After TOE guided septal puncture, a 9-French steerable guiding sheath and a multipurpose guiding catheter were positioned in the LA and a straight wire was successfully placed through the defect using 3D-TOE visualization. The wire was then exchanged to a superstiff wire and an Amplatzer valvular plug III (Abbott, Santa Clara, U.S.A.) was successfully positioned. TOE confirmed an excellent functional result with only minimal residual shunt (figure B). The postinterventional course was uneventful and despite persisting atrial fibrillation, a sudden improvement in NYHA functional class was seen and the patient was discharged three days later.
Aseptic intracardiac shunt lesions have to be considered as a rare complication in patients showing signs of heart failure after aortic valve replacement in the absence of valve deterioration. Especially unexplained volume overload should result in meticulous search for a perforation with resulting shunt lesion. When applicable, catheter-based shunt closure seems to be an excellent alternative to re-do surgery.
|
https://dgk.org/kongress_programme/jt2023/aV418.html
|