The development of an ventricular septal defect (VSD) after myocardial infarction is an infrequent but frightful complication. The hemodynamic burden of VSD is poorly tolerated and immediate action is required. We report a patient with postinfarct VSD with a device closure in the acute phase and a surgical patch repair after 20 days, leaving the occluder in place.
The patient, a previously healthy 63-year-old man, presented with an inferior myocardial infarction after 12 hours of initial pain. The right coronary artery was immediately recanalized and
a stent was placed. The next day, a new murmur was detected and an inferior VSD was diagnosed via echocardiography. Three days later, a 24 mm Amplatzer muscular VSD occluder was implanted. The defect was near the inferior papillary muscle and the mitral chordae (Fig 1a).
a stent was placed. The next day, a new murmur was detected and an inferior VSD was diagnosed via echocardiography. Three days later, a 24 mm Amplatzer muscular VSD occluder was implanted. The defect was near the inferior papillary muscle and the mitral chordae (Fig 1a).
Because of the inferior VSD location, the sheath was placed from the upper jugular vein. We attempted to place the device twice. The disk in the left ventricle was developed with different sheath angles under control of transesophageal echocardiography (TEE). We tried to avoid capturing of the mitral chordae lying next to the defect by a late opening of the device. Unfortunately the device slipped from the left into the right ventricle. In the third attempt parts of the mitral apparatus were bent with the device, but the shunt was nearly closed, and it resulted in only mild mitral insufficiency (Fig 1b).
Some days later a remaining coronary artery stenosis was treated with a stent. On follow up TEE examination we found a progressive thinning of the inferior ventricular wall. The VSD expanded and the right ventricular disk reconfigured so that the shunt still remained closed (Fig 1c). Due to this remodeling of the left ventricle, the mitral insufficiency and the concern of device dislocation the heart team decided to operate on the 20. day after the infarct.
After right atriotomy and atrial septostomy, both ventricular chambers were exposed. The antero-medial papillary muscle was slightly distorted by the deformed left-sided disk of the device. This part of the occluder was repositioned onto the septum by several transseptal stitches, leading to liberation of the mitral chordae. The residual defect was closed with a transeptally fixated patch of autologous pericardium on the right ventricular side. Postoperative TEE revealed only mild mitral insufficiency with no residual shunt (Fig 1d).
On the 6-week follow-up, the patient developed a third-degree AV Block and received a two-chamber pacemaker. After 8 weeks a partial mitral chordal rupture developed and was treated by a mitral clip implantation. The patient was discharged the same week (Fig 1e and 1f). An initial right ventricular insufficiency resolved and he was fine during the outpatient visits, currently one year after infarct.
The initial procedure of an interventional device placement successfully stabilized the VSD patient for 20 days. It was a bridging to surgery. Due to the progressive scarring with remodeling of the ventricle and distortion of the mitral apparatus the patient had to be operated. The device was left in place and fixed with an additional pericardial patch. This patient with a postinfarct VSD could be stabilised interventional und operated finally in a hybrid treatment with a good result.
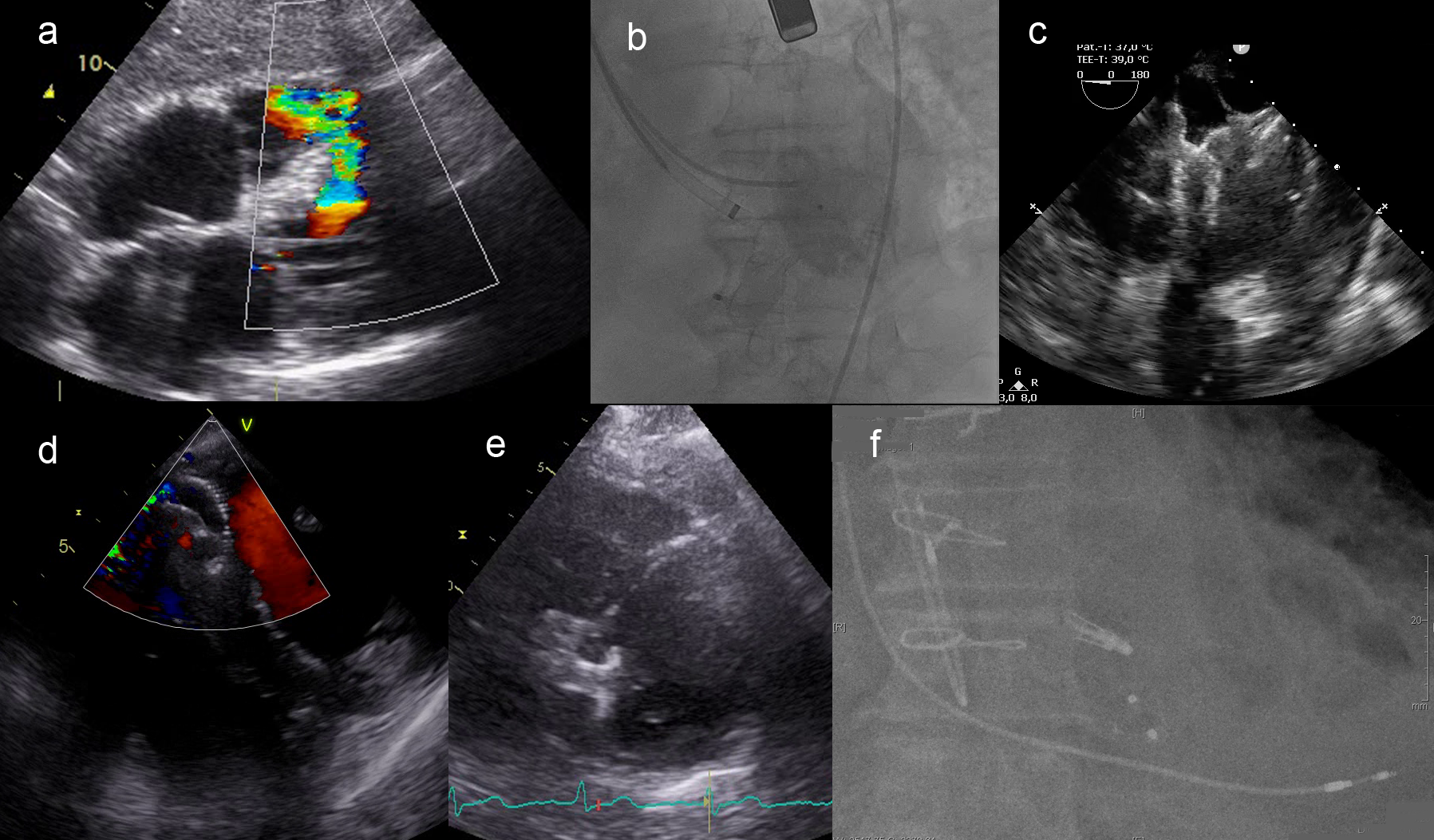
Figure 1:Postinfarct ventricular septal defect with interventional occluder closure and surgical patch fixation leaving the device in place
https://dgk.org/kongress_programme/jt2023/aV415.html