Background: Myocarditis results in a wide spectrum of symptoms. The implications of ventricular arrhythmia (VA) at initial admission are unknown. Here, we aimed to assess differences in clinical manifestation, diagnostics and long-term outcome between patients with myocarditis presenting with and without VA.
Methods: A total of 76 patients with myocarditis, confirmed by endomyocardial biopsy and/or cardiac magnetic resonance (CMR) imaging, including 38 consecutive patients with VA (44.9±2.8 years, 68.4% male) and 38 patients without VA (NVA) (38.4±2.1 years, 84.2% male) were retrospectively analyzed.
Results: In our study population, 21 (55.3%) patients presented with ventricular tachycardia, 19 (50.0%) with premature ventricular complexes and 11 (28.9%) with ventricular fibrillation as the predominant VA. Patients with VA reported syncope (55.3% vs. 2.6%; P<0.001) and palpitations (47.4% vs. 18.4%; P=0.015) more often and physical frailty (31.6% vs. 57.9%; P=0.038) and chest pain (36.8% vs. 65.8%; P=0.022) less often compared to NVA patients. Using CMR, VA patients were more likely to show late gadolinium enhancement (LGE) (94.1% vs. 68.6%; P=0.016), containing a larger amount of left ventricular myocardial volume (17.6±1.8% vs. 8.2±1.3%; P<0.001). The most common localization of LGE was mid-infero- (61.5%) and mid-anterolateral (53.8%) in the VA group, basal- (52.9%) and mid-inferolateral (47.1%) in the NVA group. Radiofrequency catheter ablation for VA was initially conducted in 9 (23.7%) patients, thereof in 7 for premature ventricular complexes, which were mainly located in the posterior left ventricle (57.1%), correlating with the site of LGE. During a follow-up of 24.9±2.5 months, 55.6% of patients remained free from any sustained VA after ablation. Left ventricular ejection fraction improved in NVA patients from baseline to follow-up (39.1±3.1% vs. 52.2±2.2%; P<0.001) but did not in those presenting with VA (46.7±2.4% vs. 50.5±1.7%; P=0.196).
Conclusions: Patients with myocarditis and VA experience different symptoms at initial admission and show LGE correlating with the origin of observed VA more frequently, with a larger extent compared to NVA patients. Therefore, CMR helps to guide catheter ablation as a reasonable therapeutic option in these patients, who may have a more serious long-term outcome than NVA patients.
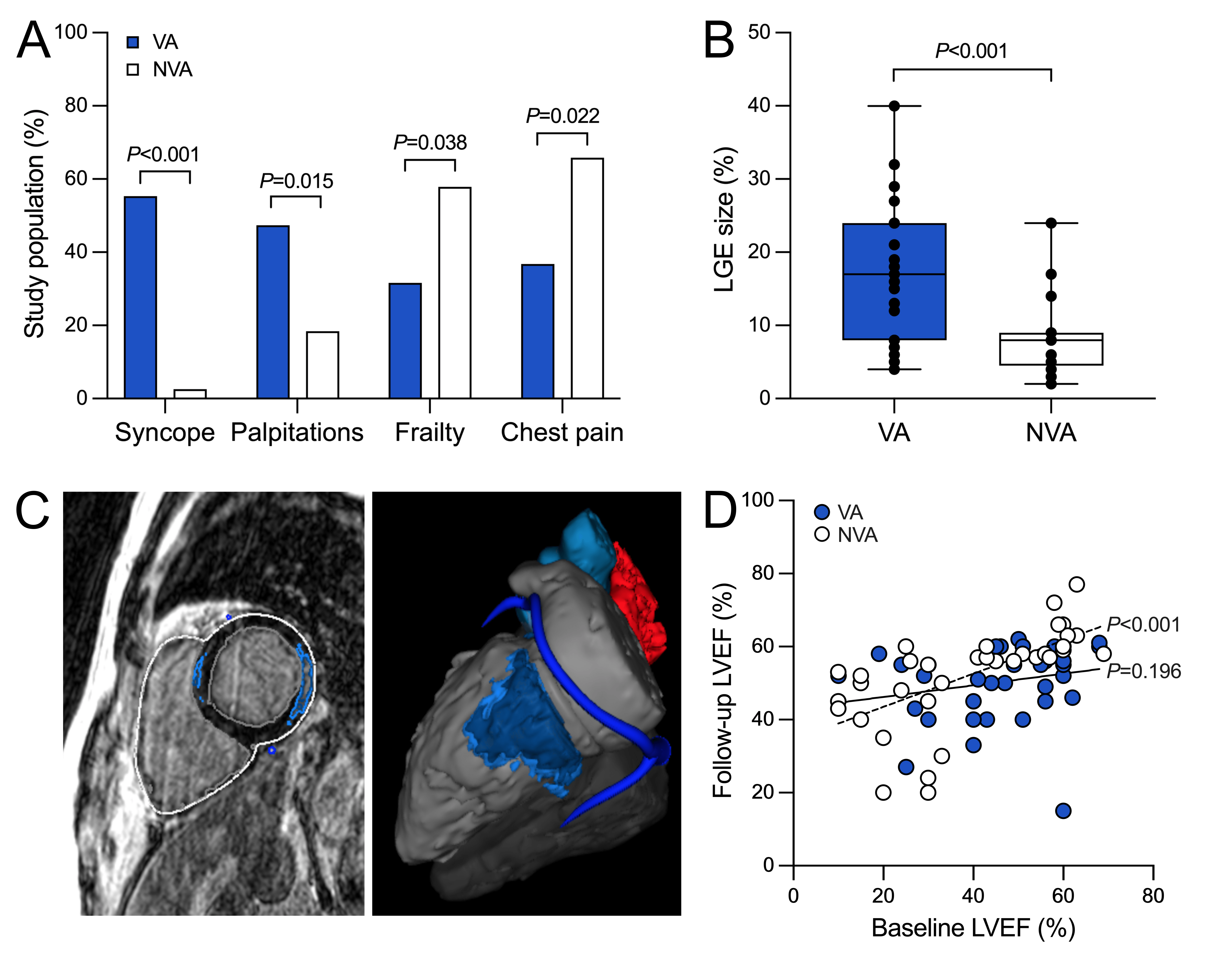
Figure: Ventricular arrhythmias in patients with myocarditis.
A, Differences in clinical symptoms for VA vs. NVA patients are illustrated. B, LGE size in % of left ventricular myocardial volume shows a larger extent in VA patients. C, Exemplary case of a patient with myocarditis who presented with ventricular tachycardia and premature ventricular complexes demonstrates how pre-procedural cardiac magnetic resonance imaging guides catheter ablation in this population. Short-axis view (left) depicts dense scar in a septal and lateral area, which was reconstructed for 3D peri-procedural guidance (right) resulting in accurate mapping and specific termination of VA. D, LVEF indicates an improvement from baseline to follow-up in the NVA group (dashed line), but not in the VA group (solid line). LGE, late gadolinium enhancement; LVEF, left ventricular ejection fraction; NVA, non-ventricular arrhythmia; VA, ventricular arrhythmia.
https://dgk.org/kongress_programme/jt2023/aV245.html