Background
Patients undergoing transcatheter aortic valve implantation (TAVI) frequently have coronary artery disease requiring percutaneous coronary intervention (PCI). The two procedures may be performed simultaneously. Combining TAVI and PCI might increase contrast agent exposure and procedure times during TAVI and may result in procedural complications, such as acute kidney injury (AKI) and bleeding. On the other hand, fusing the procedures may limit the risk associated with repeated vascular access and could prove advantageous in terms of economic efficiency. Data evaluating potential harm and benefit of combining PCI with TAVR are scarce.
Objective
The study objective was to compare concomitant or stepwise PCI in patients undergoing TAVI in terms of procedural and clinical outcomes.
Conclusions
Patients undergoing TAVI and concomitant PCI or PCI within 60 days prior to TAVI have long-term outcomes comparable to patients not undergoing PCI, despite slightly increased rates of AKI or bleeding in patients with concomitant PCI. Both, concomitant and stepwise PCI appear to be viable options if PCI is required in patients undergoing TAVI.
Methods
All 2,328 TAVI patients treated at our center between 2013 and 2018 were analyzed. Patients were split into three groups: TAVI and concomitant PCI (coPCI group), a stepwise approach with TAVI and separate PCI within 60 days prior to TAVI (swPCI group), or TAVI without PCI (noPCI group). Patients were analyzed for 3-year mortality and the Valve
Academic Research Consortium (VARC)-3 endpoints.
Academic Research Consortium (VARC)-3 endpoints.
Results
In total, 272 patients underwent TAVI and concomitant PCI, 228 patients were in the swPCI group, and 1,733 patients were in the noPCI group. Median age across the groups was 81.4 years [interquartile range, IQR, 77.1-85.6 years] and median Society of Thoracic Surgeons (STS) score was 4.0% [IQR, 2.4-6.3%], both without relevant between group differences.
The rates of the Valve Academic Research Consortium 3 (VARC-3) composite endpoints technical success (p=0.86) and device success (p=0.33) were comparable between the three groups.
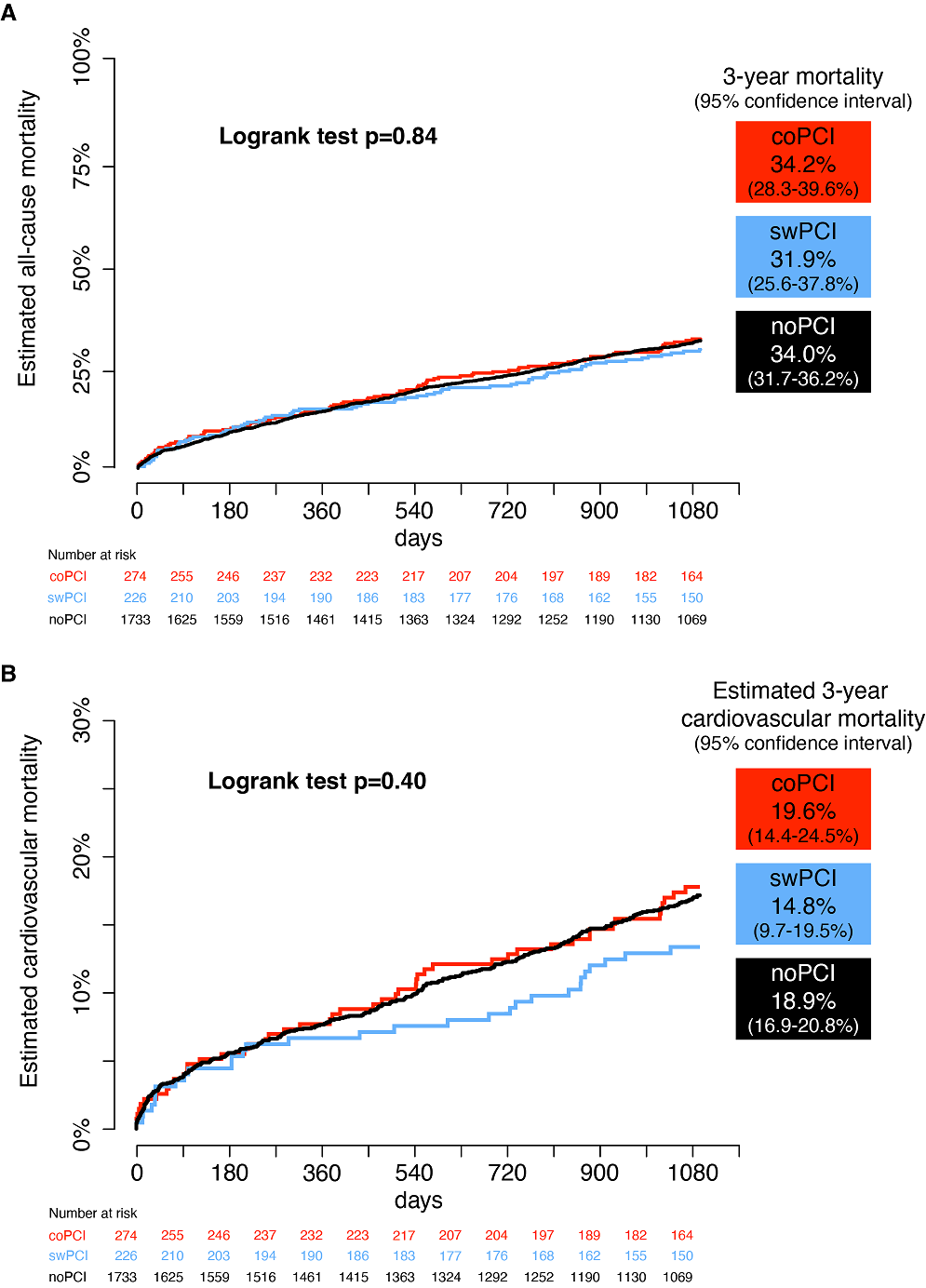
Mortality rates at 3 years were similar with 34.2% in the concomitant, 31.9% in the stepwise, and 34.0% in the no PCI group (p=0.84, Figure, panel A). Similarly, rates of cardiovascular mortality were comparable (19,6% concomitant PCI vs. 14,8% stepwise PCI vs. 18,9% no PCI, p=0.40, Figure panel B). Rates of AKI and bleeding were higher in the concomitant PCI group (17.8% vs. stepwise PCI 11.0%, p=0.04; resp. 24.8% in the concomitant group vs. 17.3% in the stepwise group, p=0.04). Conclusions
Patients undergoing TAVI and concomitant PCI or PCI within 60 days prior to TAVI have long-term outcomes comparable to patients not undergoing PCI, despite slightly increased rates of AKI or bleeding in patients with concomitant PCI. Both, concomitant and stepwise PCI appear to be viable options if PCI is required in patients undergoing TAVI.
https://dgk.org/kongress_programme/jt2023/aV1502.html