Introduction
Loeffler’s endocarditis is a rare form of restrictive cardiomyopathy characterized by eosinophilic endomyocarditis, mural thrombi, endomyocardial fibrosis and usually sustained by the presence of peripheral hypereosinophilia. Early diagnosis and prompt therapeutic interventions are usually associated with favourable disease prognosis.
Case description
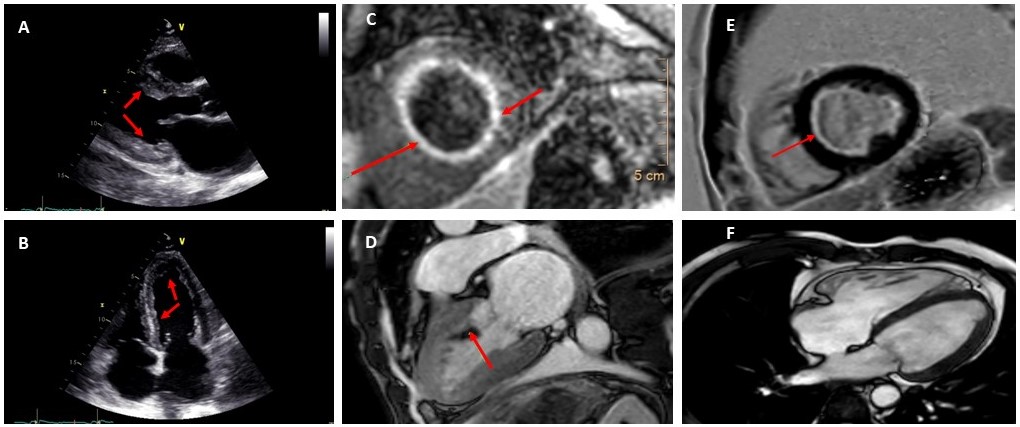
A 43-year-old male patient presented with new onset of progressive dyspnea on exertion (NYHA II) and effort intolerance. Six months earlier, he had been diagnosed with acute pericarditis and an anti-inflammatory treatment with NSAID (Ibuprofen) bought him partial pain relief. On admission, the haemogram showed anemia (4,8 mmol/l) whereas the total leucocyte and eosinophil count was normal. The C-reactive protein (62 mg/l) and NT-proBNP (11322 ng/l) and Troponin T (60 ng/l) levels were elevated. The transthoracic echocardiogram (TTE) revealed preserved global left ventricular (LV) function, a LV myocardial thickening (Panel A-B), and moderate mitral regurgitation. On physical examination, the patient showed signs of congestive heart failure.
Diagnostic work-up and discussion
Basing on the clinical and laboratory and echocardiographic findings, a cardiac magnetic resonance imaging (CMR) was performed. The latter demonstrated marked thickening of LV wall with diffused endocardial late gadolinium enhancement (LGE) at the LV walls, diagnostic of early stage of Loeffler’s endocarditis (Panel C). CMR also revealed a LV mural thrombus (Panel D). Medical therapy with high-dose oral prednisolone (1 mg/kg), anticoagulation and heart failure therapy was started.
In light of these findings, hematology/oncology was consulted. Bone marrow aspiration, cytogenetics, and molecular genetic studies ruled out malignancy or clonal eosinophilia. Culture examination of blood, urine, sputum, and stool for bacterial and parasitic infection revealed no abnormalities. Due to a medical history of intermittent arthralgia and in presence of small left-sided pleural effusion with reactive mediastinal lymphadenopathy on chest computed tomography, a workout for collagen tissue disease was conducted. This showed positivity for antinuclear antibody (ANA), anti double-stranded DNA and antihistone antibodies. Based on these findings and due to a new onset of proteinuria, extended diagnostic rheumatologic workup including renal biopsy was performed which in return showed a class III lupus glomerulonephritis. Subsequently a definite diagnosis of Loeffler’s endocarditis associated with systemic lupus erythematosus (SLE) was established and an immunotherapy with mycophenolate mofetil and hydroxychloroquine began.
At 3-month follow-up, the patient`s symptoms (NYHA I) as well as cardiac heart failure markers (NT-proBNP 3680 ng/l) improved significantly. The CMR demonstrated relevant regression of myocardial thickening revealed by LGE and complete resolution of LV thrombosis (Panel E-F respectively).
Conclusion and implication for clinical practice
This case report points to an atypical presentation of eosinophilic endomyocarditis without peripheral hypereosinophilia in the setting of SLE. Therefore, peripheral or bone marrow eosinophilia is not mandatory for the diagnosis or exclusion of Loeffler’s endocarditis. In addition, this case report shows that non-invasive imaging, mainly CMR, can provide clinical metrics in diagnostic work-up of uncertain cases.
https://dgk.org/kongress_programme/jt2023/aV1236.html