Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02180-w
|
|
Single beta-blocker or combined beta-blocker and amiodarone therapy in ICD and CRT-D patients – insights from the German DEVICE-registry
|
|
F. Wiedmann1, H. Ince2, C. Stellbrink3, T. Kleemann4, L. Eckardt5, J. Brachmann6, B.-D. Gonska7, S. Kääb8, C. A. Perings9, W. Jung10, P. Lugenbiel1, M. Hochadel11, J. Senges12, N. Frey1, C. Schmidt1
|
|
1Klinik für Innere Med. III, Kardiologie, Angiologie u. Pneumologie, Universitätsklinikum Heidelberg, Heidelberg; 2Klinik für Innere Medizin, Kardiologie und konservative Intensivmedizin, Vivantes Klinikum Am Urban, Berlin; 3Klinik für Kardiologie und intern. Intensivmedizin, Universitätsklinikum OWL, Bielefeld; 4Medizinische Klinik B, Klinikum der Stadt Ludwigshafen gGmbH, Ludwigshafen am Rhein; 5Klinik für Kardiologie II - Rhythmologie, Universitätsklinikum Münster, Münster; 6II. Medizinische Klinik - Kardiologie, Angiologie, Pneumologie, REGIOMED-KLINIKEN GmbH, Coburg; 7Klinik für Kardiologie, Intensivmedizin und Angiologie, St. Vincentius-Kliniken, Karlsruhe; 8Medizinische Klinik und Poliklinik I, LMU Klinikum der Universität München, München; 9Medizinische Klinik I, Katholisches Klinikum Lünen/Werne GmbH, Lünen; 10Klinik für Innere Medizin III: Kardiologie, Schwarzwald-Baar Klinikum, Villingen-Schwenningen; 11Statistik, IHF GmbH, Ludwigshafen am Rhein; 12Stiftung Institut für Herzinfarktforschung, Ludwigshafen am Rhein;
|
|
Background: Because of its antiarrhythmic potency and due to the lack of alternatives, amiodarone is often used for antiarrhythmic therapy in patients with ICD or CRT-D systems. To date, robust data on the safety and clinical benefit of amiodarone therapy in these patients are missing.
Objective: This study was designed to assess the periprocedural and post-procedural outcome of combined therapy with beta-blockers plus amiodarone compared to treatment with single beta-blockers in this “real life” cohort of ICD recipients of the German DEVICE registry.
Methods: 4,499 patients who underwent ICD implantation, revision, or upgrade in 49 centers participating in the German DEVICE Registry were enrolled between May 2007 and February 2014.
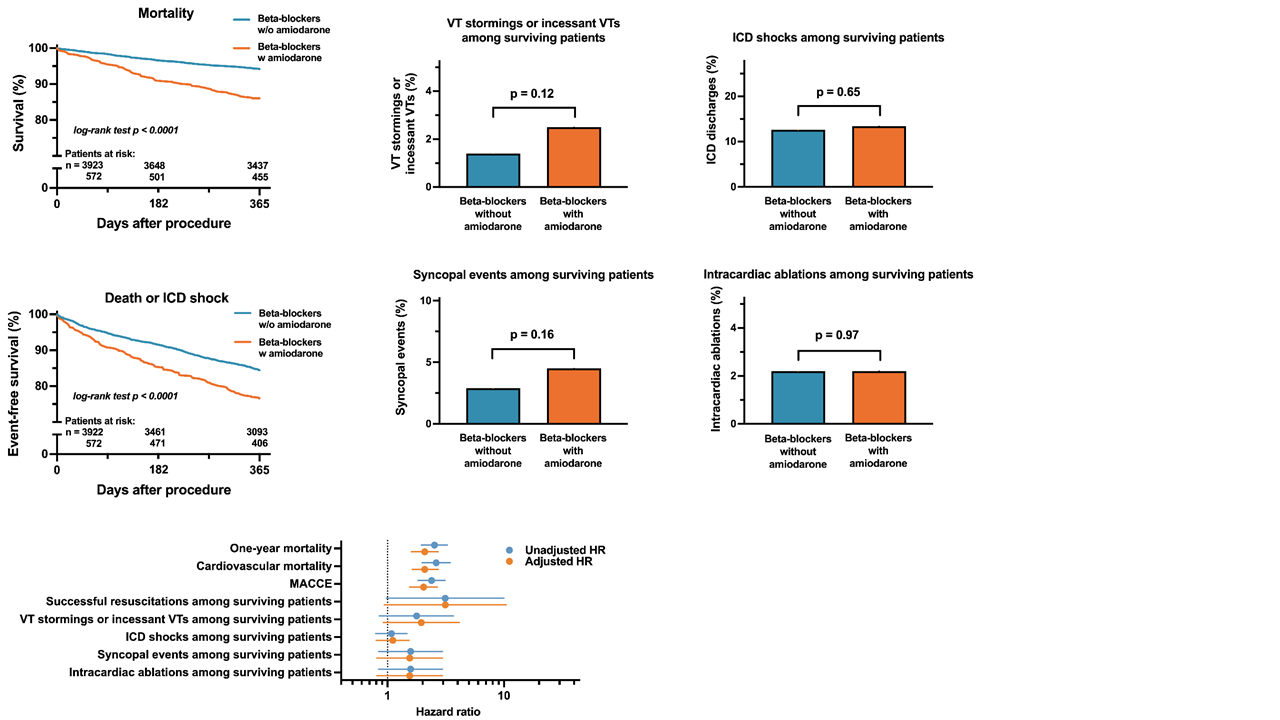
Results: Early implantation-associated complications were similar between the groups. One-year overall mortality was, however, significantly higher in the beta-blocker plus amiodarone cohort (adjusted HR 2.09; p<0.001). This was particularly pronounced in the subgroups of patients with sinus rhythm or severely impaired left ventricular function. Interestingly, amongst the surviving patients, amiodarone was not associated with a significantly reduced risk of ICD discharges or syncopal events. Further, the occurrence of ventricular tachycardia (VT) storm or incessant VTs and the number of patients scheduled for intracardiac ablation did not differ among both groups while the rate of rehospitalization was lower in the cohort with sole beta-blockers.
Conclusions: Taken together, our data suggest an increased all-cause mortality under amiodarone therapy, especially in the subgroups of patients with sinus rhythm or severely reduced left ventricular function. In surviving patients, rates of arrhythmic events were comparable.
|
https://dgk.org/kongress_programme/jt2023/aV1099.html
|