Background: Programmed ventricular stimulation may be considered for risk stratification of sudden cardiac death. Syncope appears to be helpful for identification of vulnerable patients, but data remain sparse among different populations. Here, we analyzed the prognostic value of inducible ventricular arrhythmia (VA) in patients with syncope compared to a secondary preventive indication in patients undergoing defibrillator implantation.
Methods: Among all 4,196 patients enrolled in the prospective, multi-center German Device Registry undergoing defibrillator implantation between 2007 and 2010, patients with syncope and inducible VA (n=285, 6.8%) vs. those with a secondary preventive indication (n=1,885, 45.2%) were studied. In an additional analysis of patients with inducible VA, those with vs. without (n=86, 2.1%) previous syncope were compared.
Results: Patients with a history of syncope and inducible VA (64.9±14.4 years, 81.1% male) presented less often with any structural heart disease (84.9% vs. 89.3%; P=0.030) including dilated cardiomyopathy (16.8% vs. 23.8%; P=0.009) and congestive heart failure (15.1% vs. 29.1%; P<0.001), but more frequently with hypertrophic cardiomyopathy (5.6% vs. 2.8%; P=0.010) and Brugada syndrome (2.1% vs. 0.3%; P<0.001) than patients with a secondary preventive indication (65.0±13.8 years, 81.0% male). During 1 year of follow-up, mortality (5.1% vs. 8.9%; P=0.036) and the rate of MACCE (5.8% vs. 10.0%; P=0.027) were lower in patients with syncope and inducible VA. Among patients with inducible VA, post-procedural adverse events including defibrillator shocks (16.0% vs. 15.0%; P=0.85) and rehospitalization (27.6% vs. 21.7%; P=0.37) did not differ between those with vs. without syncope.
Conclusions: Patients with syncope and inducible VA present less frequently with most cardiac comorbidities resulting in lower rates of 1-year-mortality and MACCE following defibrillator implantation compared to patients with a secondary preventive indication. Nevertheless, patients with inducible VA experience a relevant number of post-procedural adverse events not differing between those with vs. without syncope, which underlines the importance of VA inducibility, potentially irrespective of the history of a syncope.
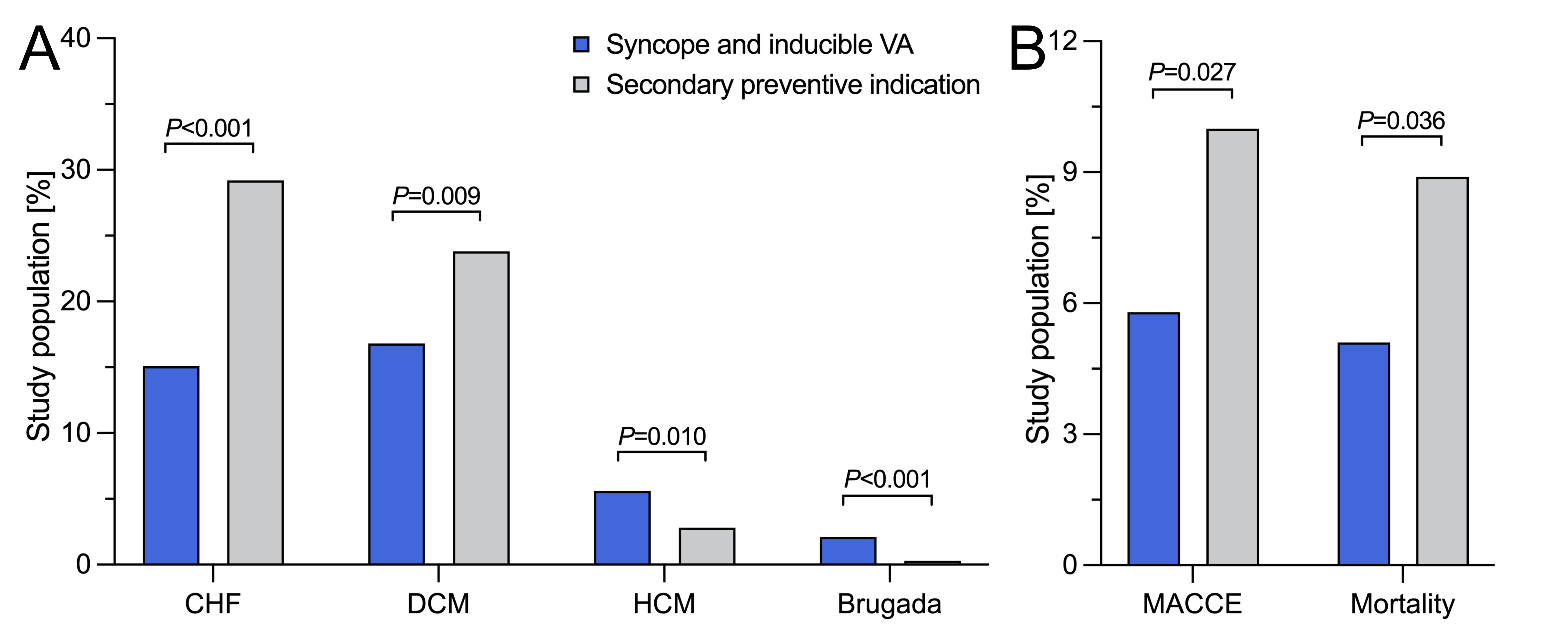
Figure: Cardiac comorbidities and post-procedural clinical outcomes during 1-year-follow-up.
Figure: Cardiac comorbidities and post-procedural clinical outcomes during 1-year-follow-up.
Patients with syncope and inducible VA undergoing defibrillator implantation A, present less often with most cardiac comorbidities and B, have lower rates of 1-year-mortality and MACCE than patients with a secondary preventive indication.
CHF, congestive heart failure; DCM, dilated cardiomyopathy; HCM, hypertrophic cardiomyopathy; MACCE, major adverse cardiac or cerebrovascular event; VA, ventricular arrhythmia.
https://dgk.org/kongress_programme/jt2023/aV1096.html