Introduction
Atrial fibrillation (AF) and heart failure (HF) often coexist and lead to increased morbidity and mortality compared to patients with AF without HF. The optimal ablation strategy in patients with HF is unclear. The aim of the study was to compare the arrythmia recurrence rates and improvement of leftventricular ejection fraction (LVEF) after pulmonary vein isolation (PVI) plus left atrial roof ablation (LARA) versus PVI alone in patients with persistent atrial fibrillation and reduced LVEF (< 55%) using cryoballoon.
Methods
In this retrospective observational study, we analyzed symptomatic patients with persistent AF and reduced ejection fraction (LVEF < 55%) undergoing cryoballoon ablation from 2014 to 2020. The primary endpoint was the first documented > 30-s arrhythmia recurrence after a 3-month blanking period. The secondary endpoints were improvements in LVEF and NYHA (“New York Heart Association”) class. For identification of independent predictors of arrythmia recurrence univariate and multivariate logistic regression were performed.
Results
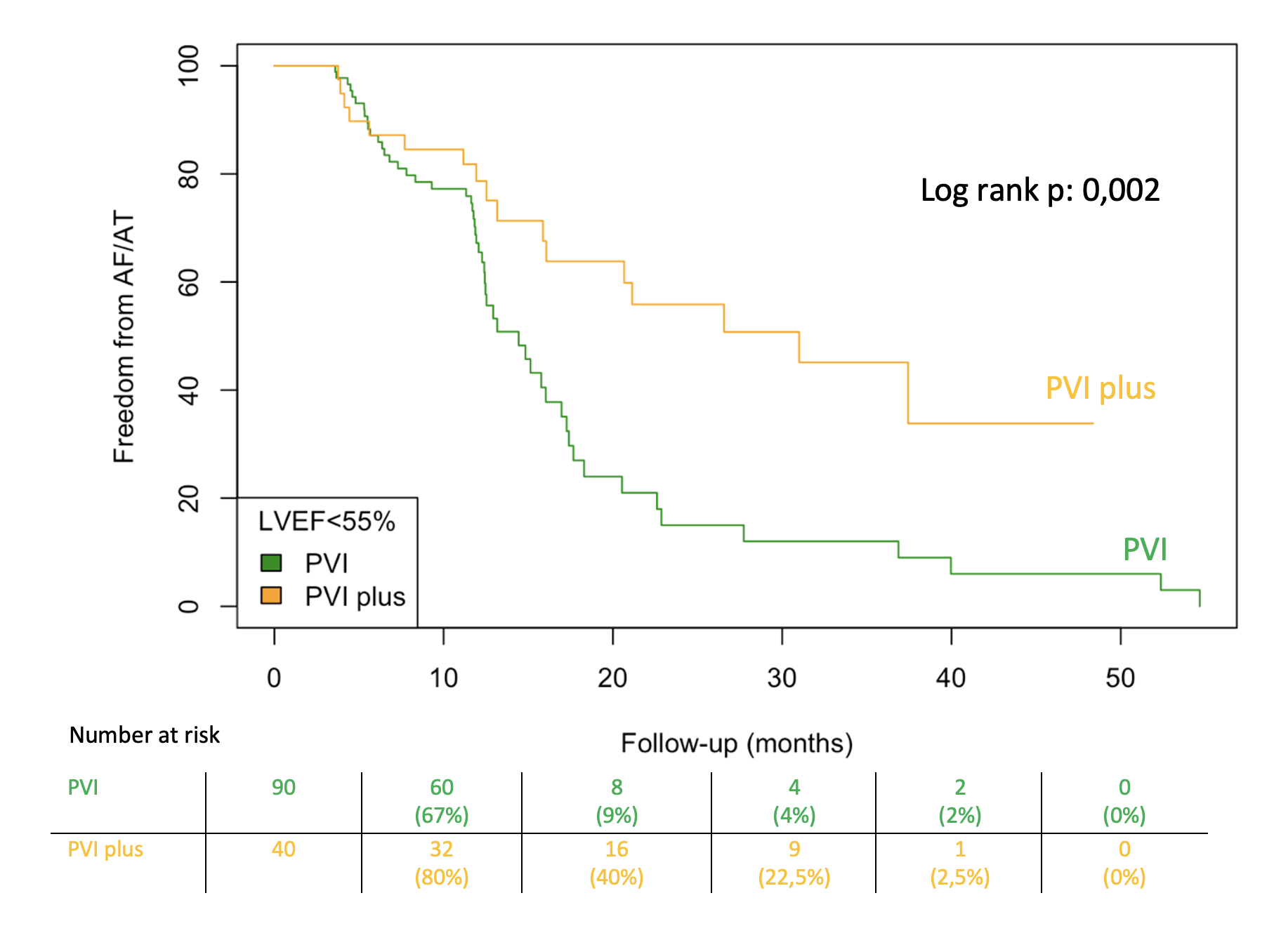
Out of 1293 consecutive patients undergoing cryoballoon ablation, 90 patients with persistent AF and reduced LVEF were treated with PVI-only strategy and 40 patients with additional LARA. Baseline characteristics, especially the prevalence of ischemic cardiomyopathy (ICM) and non-ischemic cardiomyopathy (NICM) did not differ between two groups. The median left atrial enlargement was similar between two groups (PVI-only: 26,2 cm2 versus PVI-plus: 24,3 cm2, P = 0,640). The LVEF in PVI-only group was 45% (IQR: 38-52) and in PVI-plus group 45% (IQR: 40-50), P= 0,439. During a median follow-up of 12 months (IQR: 8–16) 52 patients (57,8 %) in the PVI-only group and 17 patients (42,5%) in the PVI-plus group reached the primary endpoint. The recurrence-free survival rate was significantly higher in the PVI-plus group compared with the PVI-only group (log-rank P = 0.002). After univariate analysis following parameters were associated with arrythmia recurrence: male sex (HR = 0,45, P = 0,049) and LARA (HR = 0,34, P = 0,026). Multivariate analysis revealed LARA (HR = 0.43, P = 0.004) as the only significant predictor of outcome. Both groups have similar improvements in NYHA class (-0,52 ± 0,85 versus -0,58 ± 0,84, P = 0,850) and in LVEF (12% (IQR: 5-20) versus 10% (IQR: 2-18), P = 0,190).
Conclusions
A significant difference in arrhythmia recurrence rates between the two groups was observed. We found similar improvements in LVEF and NYHA class in both groups during follow-up. Additional left atrial roof ablation using cryoballoon is an effective treatment in patients with persistent atrial fibrillation and heart failure compared with PVI alone, although LARA has no additional impact on improvement in LVEF.
https://dgk.org/kongress_programme/jt2023/aP873.html