Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02180-w
|
|
The role of the biomarker NT-proBNP to predict or exclude increased left ventricular enddiastolic filling pressure – insights from an all-comers registry study
|
|
M. Mendez-Braeutigam1, M. Lehmann1, J. Urban1, S. Schulze2, J. Buschenhenke1, K. Nobis-Joachim1, C. Friedrich3, K. Huenges3, A. Haneya3, J. Strotmann1
|
|
1I. Medizinische Klinik, Städtisches Krankenhaus Kiel GmbH, Kiel; 2Zentrallabor, Städtisches Krankenhaus Kiel GmbH, Kiel; 3Klinik für Herz- und Gefäßchirurgie, Universitätsklinikum Schleswig-Holstein, Kiel;
|
Background: Heart failure diagnosis especially in patients with preserved ejection fraction (HFpEF) is complex. One important biomarker to rule in or rule out HFpEF is NT-proBNP. We sought to investigate the role of NT-proBNP to predict increased left ventricular enddiastolic pressure (LVEDP) (the physiologic hallmark of HFpEF) in patient groups with systolic heart failure and EF < 50% and patients with diastolic heart failure (HFpEF) with an EF ≥ 50%. Methods: We included over 1000 consecutive patients who underwent left heart catheterization for different clinical indications in an all-comers registry. For those patients invasive measurements of LVEDP were done including assessment of NT-proBNP at the same time. Within 24 hours of the invasive procedure a full echocardiography was performed. All patients gave written informed consent to participate in the study. Results: A total number of 990 patients were included in the analysis. The patients were all at NYHA I to IV stages. A total number of 182 patients had an EF < 50% (EF 37% (26%;43%)) and 808 patients had an EF ≥ 50% (EF 62% (58%;66%)) (median values plus the 25. and 75. percentile). The patient group with an EF < 50% included 26.9% of patients with atrial fibrillation in contrast to 11.5% of patients with atrial fibrillation in the HFpEF group (p<0.001). The median NT-proBNP level for the group with an EF < 50% was significantly higher than the median NT-proBNP level for the patient group with an EF ≥ 50% ( 1635 pg/ml vs. 171 pg/ml, p < 0.001). After subdividing both patient groups into NYHA classes I to IV we could not see a significant difference of NT-proBNP levels between the NYHA classes in the patient group with reduced EF < 50% . In contrast, in the patient group with an EF ≥ 50% there was a significant increase in NT-proBNP levels comparing NYHA class I and II with all other NYHA classes. There was no difference in NT-proBNP comparing class III with class IV. For the patients with an EF < 50% the correlation between LVEDP and NT-proBNP was highly significant but with a low correlation-coefficient (Spearman’s rank correlation coefficient: 0,304; p < 0.001). The patient group with an EF ≥ 50% also had a highly significant correlation of LVEDP and NT-proBNP but again with a low correlation coefficient (0.231; p < 0.001) (Fig 1). The positive predictive value of NT-proBNP levels ≥ 125 pg/ml for an LVEDP ≥ 15 mmHg was 62,4% and the negative predictive value to rule out LVEDP ≥ 15 mmHg was 66,7% in patients with reduced ejection fraction. Looking at patients with HFpEF (EF ≥ 50%) the positive predictive value of NT-proBNP ≥ 125 pg/ml for an LVEDP ≥ 15 mmHg was 57,9 % and the corresponding negative predictive value to rule out LVEDP ≥ 15 mmHg was 60%. A total number of 138 out of 406 patients with preserved EF ≥ 50% showed normal NT-proBNP levels < 125 pg/ml in the presence of elevated LVEDP ≥ 15 mmHg (Fig1, red box).
Conclusion: NT-proBNP levels have a significant correlation to LVEDP. They are also significantly different comparing patients with EF < or ≥ 50%, or patients with normal and increased LVEDP. However, with a negative predictive value of 60% there are at least some limitations to use NT-proBNP concentrations in the individual patient to predict an increased LVEDP in HFpEF. 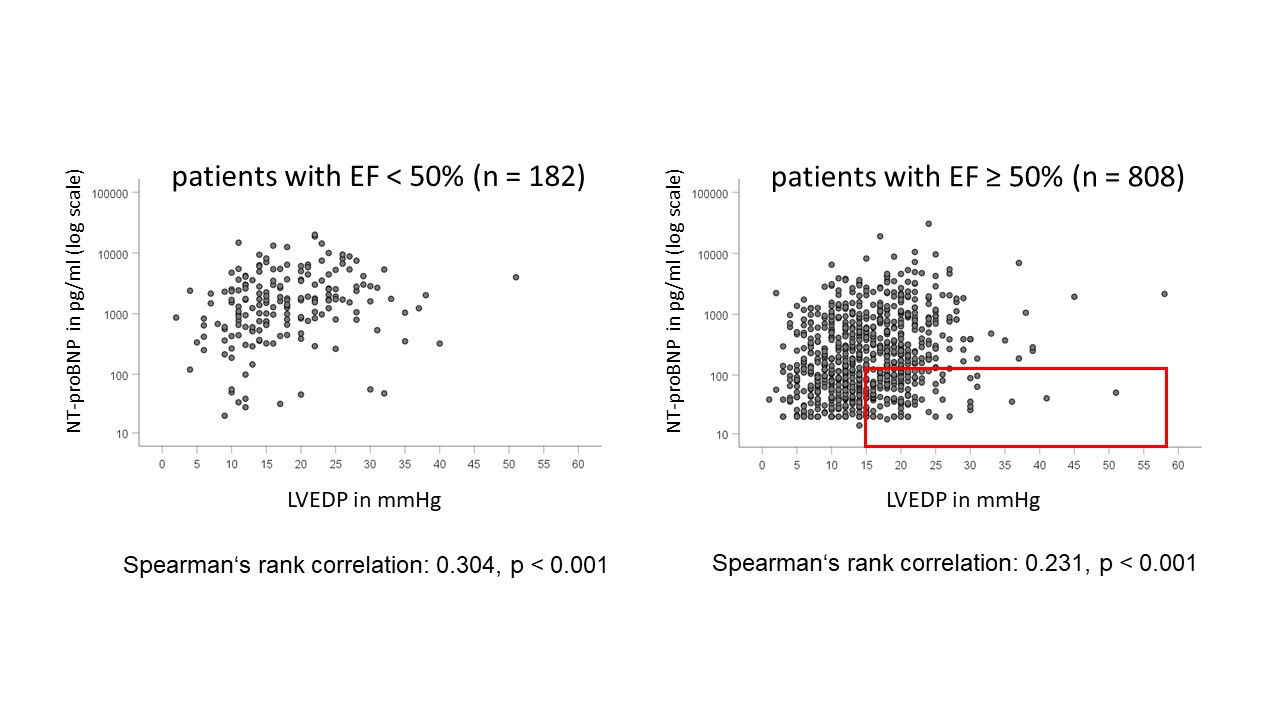
|
https://dgk.org/kongress_programme/jt2023/aP2103.html
|