Background:
Heart failure with preserved ejection (HFpEF) is a growing health care problem and is associated with high morbidity and mortality. So far, transcatheter edge-to-edge-repair (TEER) of mitral valve regurgitation (MR) in patients with heart failure with reduced ejection fraction (HFrEF) has been the focus of large trials. However, the effect of interventional treatment of MR in patients with HFpEF is largely unknown. Therefore, we seek to investigate the impact of HFpEF according to established diagnostic scores in patients undergoing TEER regarding symptom burden, exercise capacity and prognosis.
Methods and Results:
HFpEF criteria of H2FPEF-Score, HFAPEFF-Score and European Society of Cardiology (ESC) guidelines were assessed in 182 patients undergoing TEER with LV-EF >50%. Mean age was 80±6 years. 60% of patients were female and mean BMI was 26±5 kg/m2.
HFpEF was diagnosed in 181 patients (N=181, 100%) according to ESC guideline definition, in 152 (N=181, 84%) according to HFA-PEFF score, and 81 (N=140, 58%) according to H2FPEF score.
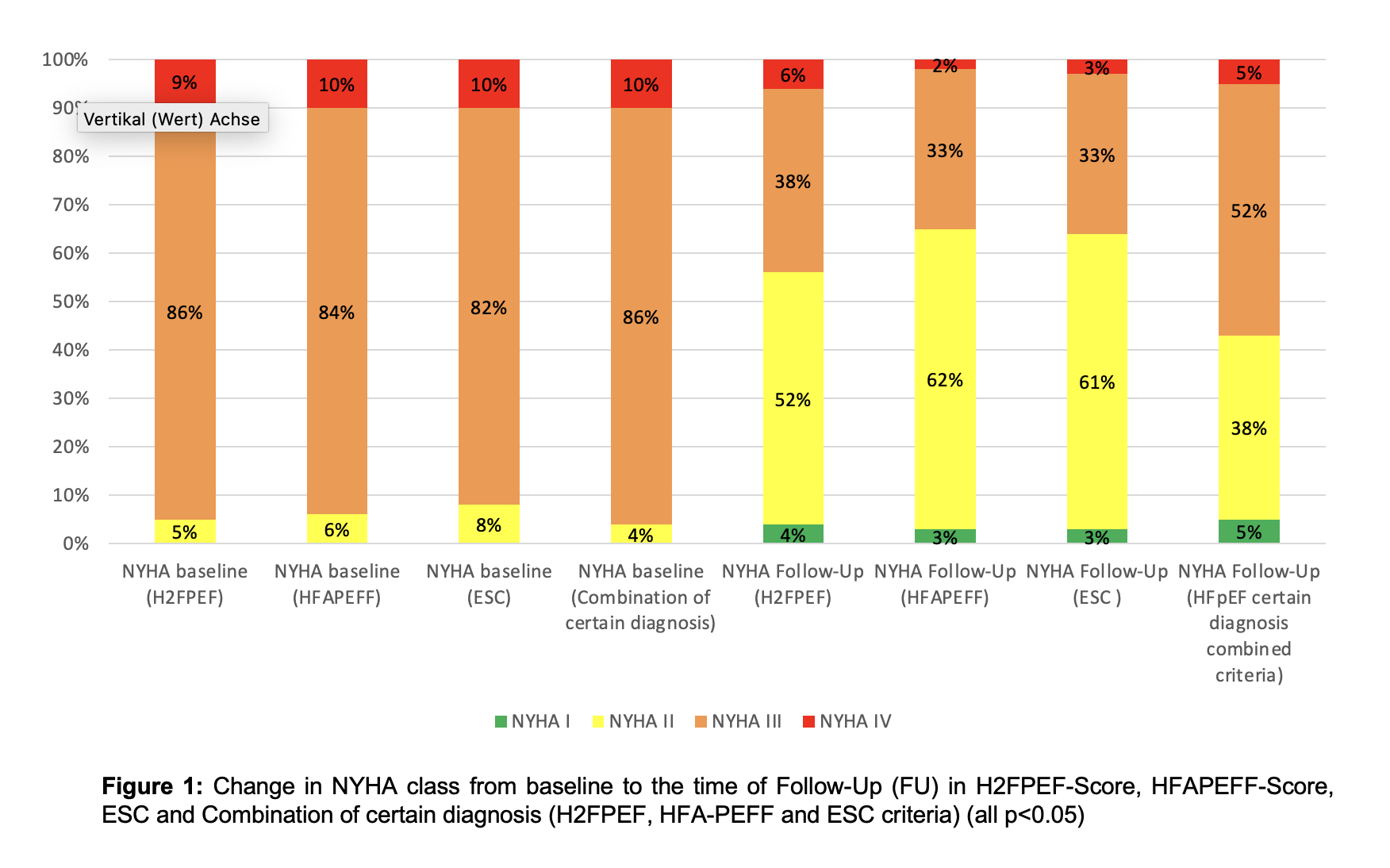
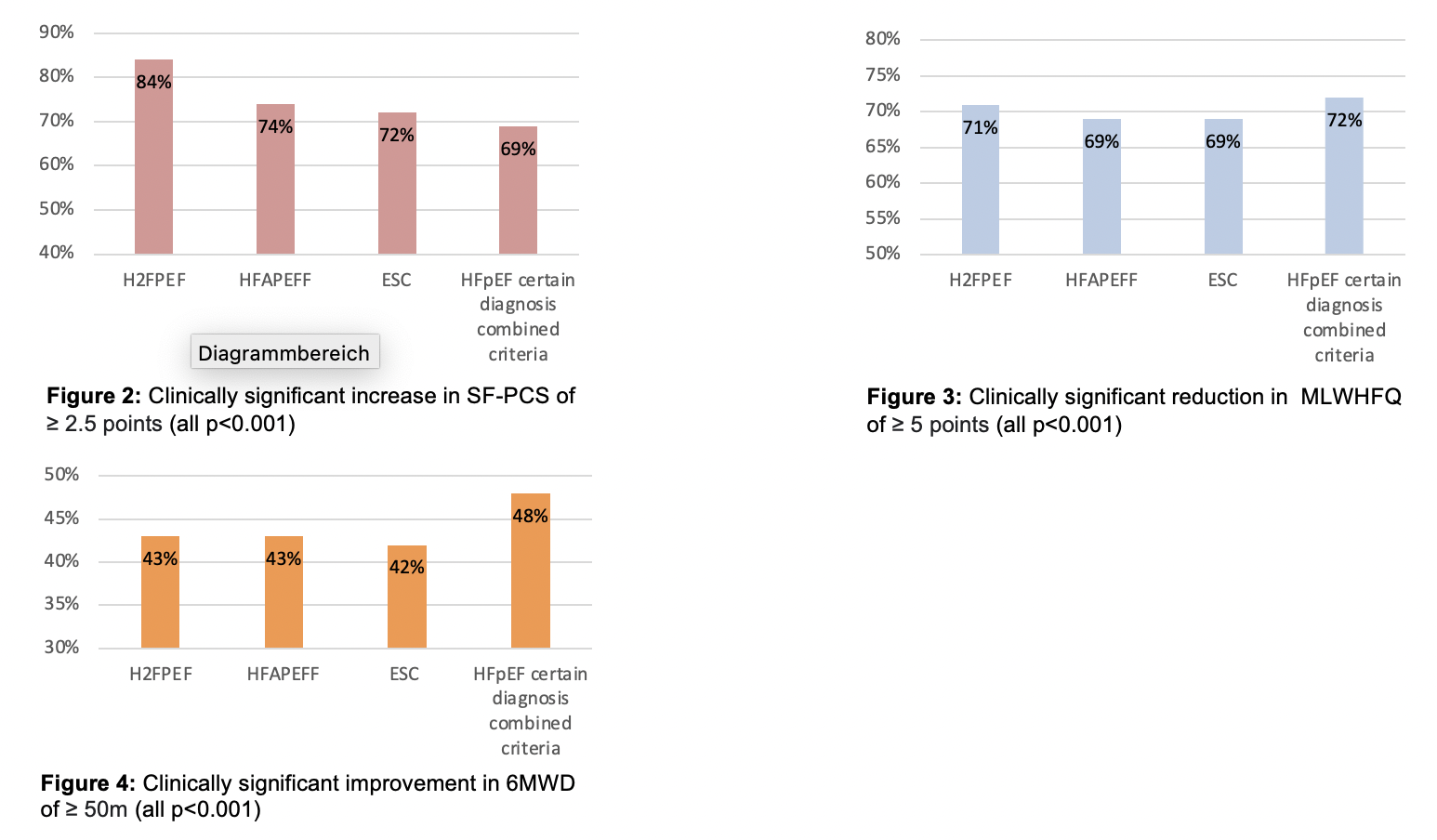
MR reduction to grade <=2+ was achieved in 69%, 64% and 65% of patients with H2FPEF, HFA-PEFF, and ESC diagnosis, respectively. After 30 days, NYHA class improved significantly (I/II class) from 4 to 56% in patients with HFpEF according to H2FPEF, from 6% to 65% according to HFA-PEFF, and from 8% to 64% according to ESC definition (all p<0.05) (Figure 1). Quality of life was measured with the Minnesota Living with Heart Failure Questionnaire (MLWHFQ) and Short Form-36 Physical Component Summary Score (SF-PCS); a similar clinically relevant improvement was evident in all groups (Figure 2 and 3). Furthermore, in 6-minutes-walk distance (6MWD) we could observe a similar amount of clinically relevant enhancement in functional capacity of at least 50 m in all groups (Figure 4). Subgroup analysis did not reveal any significant differences by MR aetiology (primary vs secondary).
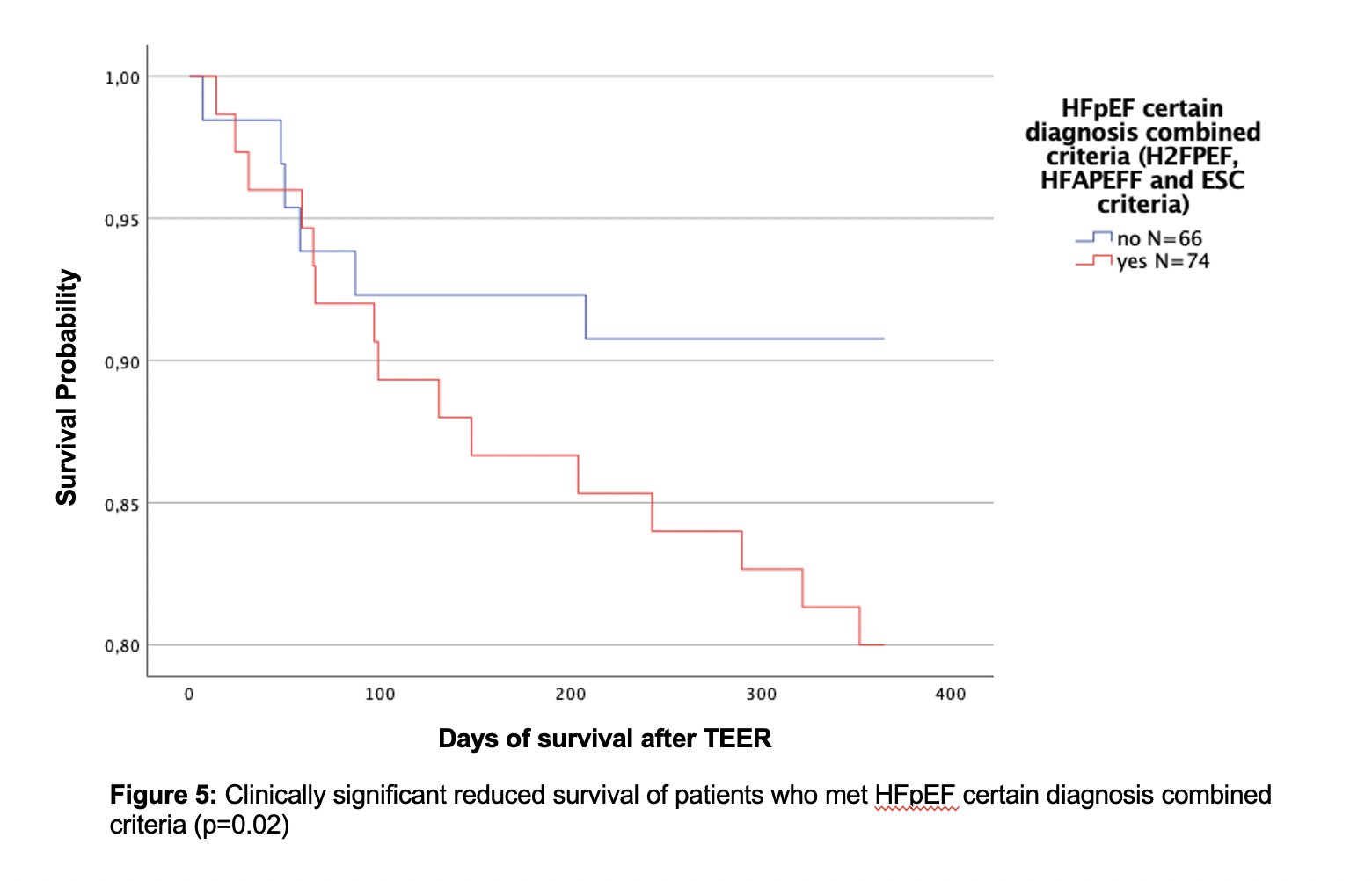
However, the combination of all three scores (H2FPEF, HFA-PEFF and ESC certain diagnosis criteria) revealed a higher risk subgroup. Those patients (N=74) had a higher long-term mortality risk compared to the others (N=66) (HR 2.6, 95%CI [1.15-5.81], p=0.02) (Figure 5). Despite the reduced survival probability there was an improvement in NYHA class (I/II) from 4% to 57%. A clinically relevant improvement of MLWHFQ and SF-PCS was achieved in 72% and 69% respectively. Consequently, we could also see a clinically relevant amelioration in 6MWD in 48% of this subgroup.
Conclusion:
These data suggest that TEER is an effective therapy in patients with HFpEF to reduce symptomatic burden and improve exercise capacity, independent of the diagnostic criteria applied. Furthermore, patients who met the combined criteria of all three scores had also relevant clinical improvement, although they were associated with worse prognosis. Randomized trials are warranted, particularly in the context of secondary MR, to examine the effect of TEER in patients with HFpEF.
https://dgk.org/kongress_programme/jt2023/aP1791.html