Clin Res Cardiol (2023). https://doi.org/10.1007/s00392-023-02180-w
|
|
Symptomatic vs. non-symptomatic device-related thrombus after LAAC– a sub-analysis from the multicenter EUROC-DRT registry
|
|
V. O. Vij1, I. Cruz-Gonzalez2, R. Galea3, K. D. Piayda4, D. Nelles1, L. Vogt1, S. Gloekler5, M. Fürholz3, B. Meier3, L. Räber3, G. O'Hara6, D. Arzamendi7, V. Agudelo7, L. Asmarats7, X. Freixa8, E. Flores-Umanzor8, O. De Backer9, L. Sondergaard9, L. Nombela-Franco10, A. McInerney10, K. Korsholm11, J. E. Nielsen-Kudsk11, S. S. Afzal12, T. Zeus12, F. K. Operhalski13, B. Schmidt14, G. Montalescot15, P. Guedeney15, X. Iriart16, N. Miton16, J. Saw17, T. Gilhofer18, L. Fauchier19, E. Veliqi20, F. Meincke21, N. Petri22, P. Nordbeck23, R. Gonzalez-Ferreiro2, D. L. Bhatt24, A. Laricchia25, A. Mangieri25, H. Omran26, J. W. Schrickel1, J. Rodes-Cabau6, G. Nickenig1, H. Sievert4, A. Sedaghat1
|
|
1Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Bonn; 22) University Hospital of Salamanca, CIBER CV, Salamanca, ES; 3Klinik und Poliklinik für Kardiologie, Inselspital - Universitätsspital Bern, Bern, CH; 4CVC Rhein-Main GmbH, Frankfurt am Main; 5Zentrum Innere Medizin · Medizinische Klinik I, Klinikum Hochrhein GmbH, Waldshut; 6Quebec Heart & Lung Institute, Laval University, Quebec, CA; 7Cardiology, Hospital de la Santa Creu i Sant Pau, Barcelona, ES; 8Cardiology, Hospital Clinic Barcelona, Barcelona, ES; 9Cardiology, Rigshospitalet Copenhagen, Copenhagen, DK; 10Cardiology, Hospital Clinico San Carlos Madrid, Madrid, ES; 11Cardiology, Aarhus University Hospital, Aarhus, DK; 12Klinik für Kardiologie, Pneumologie und Angiologie, Universitätsklinikum Düsseldorf, Düsseldorf; 13Medizinische Klinik I, Main-Kinzig-Kliniken GgmbH, Gelnhausen; 14Agaplesion Markus Krankenhaus, Frankfurt am Main; 15Cardiology, Pitié-Salpêtrière Hospital, Paris, FR; 16Cardiology, University Hospital Bordeaux, Paris, FR; 17Vancouver General Hospital, Vancouver, CA; 18Kardiologie, Stadtspital Triemli Zürich, Zürich, CH; 19Cardiology, University Hospital Tours, Tours, FR; 20Kardiologie, Asklepios Klinik St. Georg, Hamburg; 213. Med. Abteilung - Kardiologie, Pneumologie und Internistische Intensivmedizin, Asklepios Klinik Altona, Hamburg; 22Medizinische Klinik und Poliklinik I, ZIM Kardiologie, Universitätsklinikum Würzburg, Würzburg; 23Medizinische Klinik und Poliklinik I, Universitätsklinikum Würzburg, Würzburg; 24Cardiology, Brigham and Women’s Hospital Heart and Vascular Center, Boston, US; 25Department of Biomedical Sciences, Humanitas University, Pieve Emanuele, Italy and Humanitas Research Hospital IRCCS, Rozzano, IT; 26Innere Medizin / Kardiologie, GFO Kliniken Bonn, Bonn;
|
|
BACKGROUND
Device-related thrombus (DRT) after left atrial appendage closure (LAAC) is a common complication and is associated with adverse outcome, i.e. ischemic stroke or systemic embolism (SE). However, data on predictors of stroke/SE in the context of DRT are limited.
AIMS
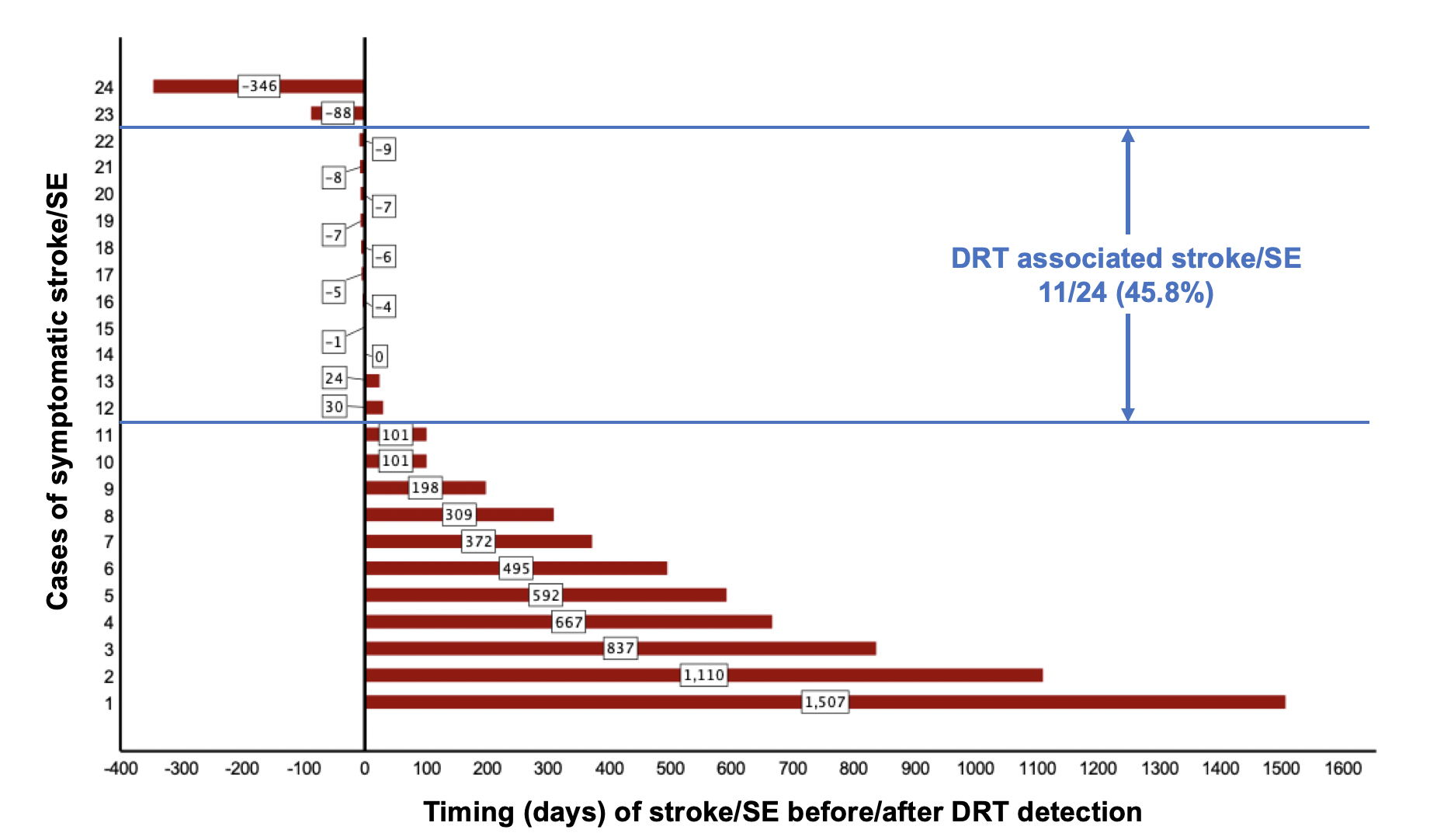
This study aimed to identify predisposing factors for stroke/SE in patients that develop DRT after LAAC. Also, temporal connection of stroke/SE to DRT diagnosis was analyzed.
METHODS
The multicenter EUROC-DRT registry included 176 patients, in whom DRT after LAAC were diagnosed. Patients with symptomatic DRT, defined as stroke/SE in the context of DRT diagnosis, were compared against patients with non-symptomatic DRT. Baseline characteristics, anti-thrombotic regimens, device position, and timing of stroke/SE were compared.
RESULTS
Stroke/SE occurred in 25/176 (14.2%) patients diagnosed with DRT (symptomatic DRT). Stroke/SE occurred after a median of 198 days (IQR: 37-558) after LAAC. In 45.8% stroke/SE occurred within one month before/after DRT diagnosis (DRT-related stroke). Patients with symptomatic DRT had lower left ventricular ejection fractions (50.0±9.1% vs. 54.2±11.0%, p=0.03) and higher rates of non-paroxysmal atrial fibrillation (84.0% vs. 64.9%, p=0.06). Other baseline parameters and device position were not different. Most ischemic events occurred among patients with single antiplatelet therapy (50%), however, stroke/SE was also observed under dual antiplatelet therapy (25%) or oral anticoagulation (20%).
CONCLUSION
Stroke/SE are documented in 14.2% and occur both in close temporal relation to the DRT finding and chronologically independently therefrom. Evidence of risk factors remains scarce, putting all DRT patients at substantial risk for stroke/SE. Further studies are necessary to minimize the risk of DRT and ischemic events.
Figure 1) Timing of stroke/SE from DRT diagnosis in each reported case of symptomatic DRT
|
https://dgk.org/kongress_programme/jt2023/aP1277.html
|