A 77-year-old female patient has been referred for ablation of symptomatic typical atrial flutter. The MR-guided procedure under conscious sedation was initiated in the scanner as a part of an MR-only workflow. After placement of 2 venous sheaths (Fr. 11) in the left femoral vein, a series of balanced steady state free precession (bSSFP) localizers in sagittal and coronal plane were acquired. Subsequently, introduction of 2 catheters (both Fr. 9) was performed under direct visualization using active tip tracking with automatic slice positioning. After positioning of the first catheter in the inferior vena cava (IVC), advancement of the second catheter at 45 cm was not possible and the tip could not be tracked by the MR scanner. To ascertain the position of the catheter a stack of bSSFP images in the coronal plane was acquired (11:32). Despite correct position in the bifurcation of the IVC, the resistance persisted with no further advancement possible. Another stack in the coronal plane was acquired (11:38) and appearance of retroperitoneal mass could be shown. A stack of bSSFP images in the axial plane (11:41) raised a suspicion of the anterior IVC perforation with the tip of the second catheter. As the condition of the patient remained stable, the decision to transport the patient to the CT-scanner was made. The CT scan (11:58) with both catheters left in situ confirmed the suspected venous perforation and showed a retroperitoneal hematoma with no signs of active bleeding in neither arterial nor venous phase. The catheter removal (13:01) was performed under fluoroscopic control with a guidewire and 24 x 60 mm balloon placed through the contralateral femoral vein. As there were no signs of active bleeding upon injection of contrast agent, complete removal of the material and subsequent venous access closure were performed. There was no need for vasopressor or blood products use. The patient recovered without sequelae and was discharged after two days of in-patient monitoring. The oral anticoagulants (Edoxaban 60 mg once daily) were restarted on the fifth day. This was deemed safe as the patient was in sinus rhythm during the stay.
Performing MR-guided electrophysiological procedures necessitates careful revision of the safety procedures that are commonplace in the traditional EP lab. This case demonstrates the feasibility of prompt diagnosis and management of complications regarding vascular access and catheter advancement in the MR environment.
Adding more imaging planes or adjusting the intensity of the hyperintense tip-signal could prove useful in facilitating catheter insertion during active tracking.
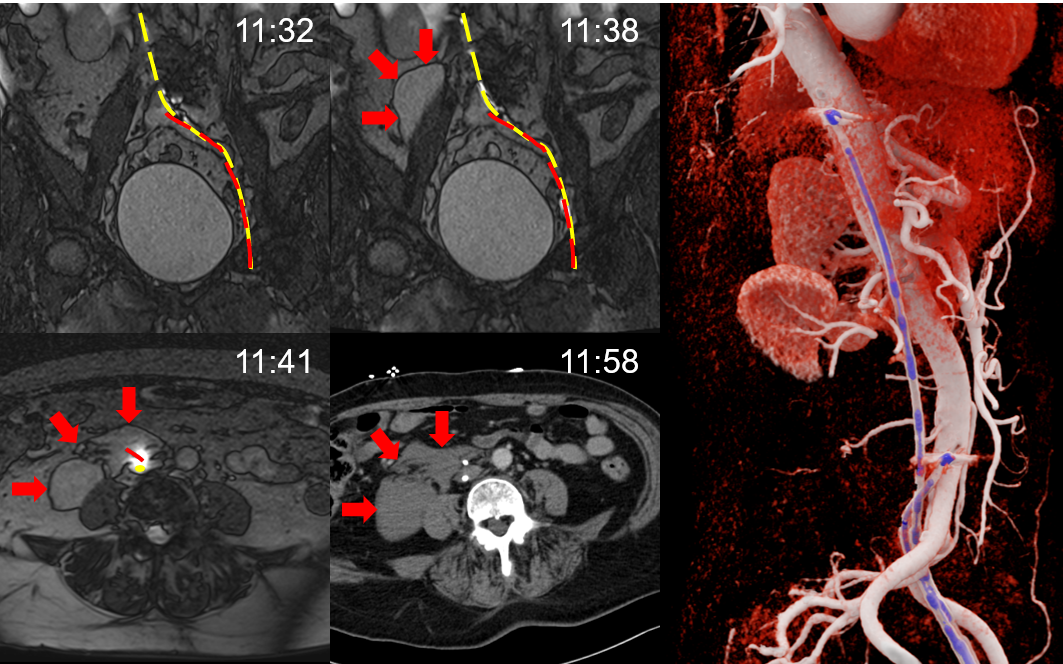
Fig. 1: upper row, left to right – coronal planes, initial position and retroperitoneal mass adjacent to right psoas major; lower row, left to right – axial planes, perforation of the anterior IVC with retroperitoneal hematoma, MR and corresponding CT images with time of acquisition; right – reconstruction of CT-angiography showing contrasted aorta and catheter position in the IVC (IVC not shown)
Fig. 1: upper row, left to right – coronal planes, initial position and retroperitoneal mass adjacent to right psoas major; lower row, left to right – axial planes, perforation of the anterior IVC with retroperitoneal hematoma, MR and corresponding CT images with time of acquisition; right – reconstruction of CT-angiography showing contrasted aorta and catheter position in the IVC (IVC not shown)
https://dgk.org/kongress_programme/jt2022/aP1919.html