Clin Res Cardiol (2022). https://doi.org/10.1007/s00392-022-02002-5
|
|
Left ventricular unloading in patients with cardiogenic shock and veno-arterial extracorporeal membrane oxygenation (ECMELLA) improves both mortality and neurological outcome.
|
|
B. Beer1, A. Goßling1, P. Kirchhof1, S. Blankenberg2, P. M. Becher3, A. Bernhardt4, D. Eckner5, M. Eden6, I. Eitel7, D. Frank8, N. Frey6, T. Graf7, D. Kupka8, U. Landmesser9, N. Majunke10, O. Maniuc11, S. Möbius-Winkler12, C. Noel13, P. Nordbeck14, M. Orban15, M. Pauschinger5, H. Reichenspurner16, M. Sandri10, C. Schulze12, R. H. G. Schwinger17, A. Aksoy18, C. Skurk9, L. Szczanowicz10, H. Thiele10, F. Tietz10, L. Wechsler17, B. Schrage1, D. Westermann3
|
|
1Klinik für Kardiologie, Universitäres Herz- und Gefäßzentrum Hamburg GmbH, Hamburg; 2Klinik für Kardiologie, Universitäres Herz- und Gefäßzentrum UKE Hamburg GmbH, Hamburg; 3Allgemeine und Interventionelle Kardiologie, Universitäres Herz- und Gefäßzentrum Hamburg GmbH, Hamburg; 4Klinik für Herz- und Gefäßchirurgie, Universitäres Herz- und Gefäßzentrum UKE Hamburg, Hamburg; 5Klinik für Innere Medizin 8, Schwerpunkt Kardiologie, Universitätsklinik der Paracelsus Medizinischen Privatuniversität, Nürnberg; 6Klinik für Innere Med. III, Kardiologie, Angiologie u. Pneumologie, Universitätsklinikum Heidelberg, Heidelberg; 7Medizinische Klinik II / Kardiologie, Angiologie, Intensivmedizin, Universitätsklinikum Schleswig-Holstein, Lübeck; 8Klinik für Innere Medizin III, Kardiologie, Angiologie und Intensivmedizin, Universitätsklinikum Schleswig-Holstein, Kiel; 9CC 11: Med. Klinik für Kardiologie, Charité - Universitätsmedizin Berlin, Berlin; 10Klinik für Innere Medizin/Kardiologie, Herzzentrum Leipzig - Universität Leipzig, Leipzig; 11Med. Klinik und Poliklinik I, Klinische Elektrophysiologie, Universitätsklinikum Würzburg, Würzburg; 12Klinik für Innere Medizin I - Kardiologie, Universitätsklinikum Jena, Jena; 13Christian-Albrechts-Universität zu Kiel, Kiel; 14Medizinische Klinik und Poliklinik I, Universitätsklinikum Würzburg, Würzburg; 15Medizinische Klinik und Poliklinik I, LMU Klinikum der Universität München, München; 16Klinik und Poliklinik für Herz- und Gefäßchirurgie, Universitäres Herz- und Gefäßzentrum Hamburg GmbH, Hamburg; 17Medizinische Klinik II, Kardiologie, Kliniken Nordoberpfalz AG, Weiden i. d. Oberpfalz; 18Medizinische Klinik und Poliklinik II, Universitätsklinikum Bonn, Bonn;
|
|
Aims: Cardiogenic shock (CS) remains a condition with high mortality. Currently, mechanical circulatory support devices (MCS) are investigated as a ‘bridge to recovery therapy’. A recent approach is the combination of a VA-ECMO with the left ventricular (LV) unloading device Impella® to prevent typical VA-ECMO complications (“ECMELLA”). In recent cohort studies the ECMELLA approach proved to reduce mortality compared to VA-ECMO alone. However, little is known about the neurological outcome and quality-of-life in survivors. This study aimed to identify predictors of good neurological outcome in patients treated with ECMELLA and compare them to predictors for 30-day survival.
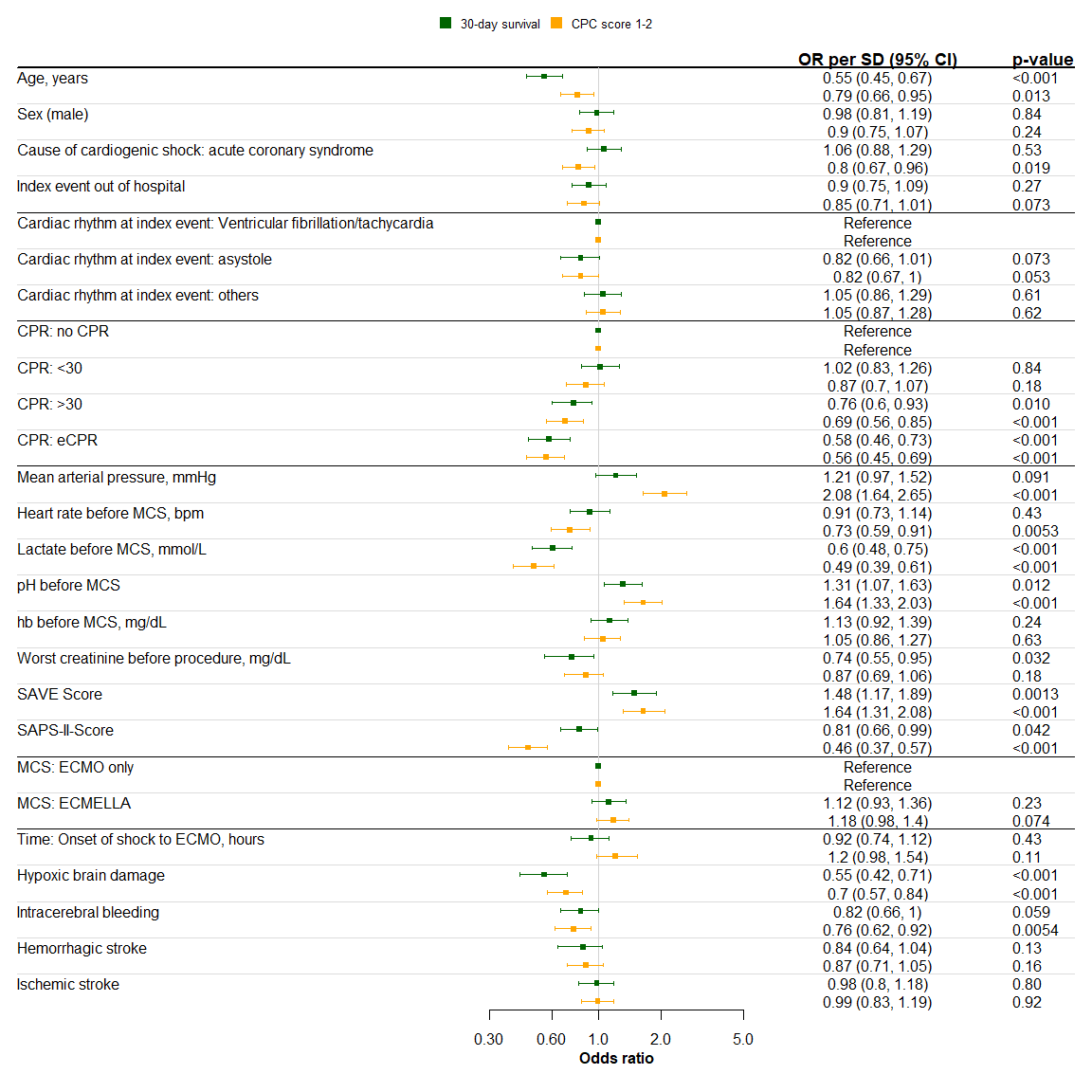
Methods and results: 501 patients with CS unselected for its aetiology, who were treated with either VA-ECMO alone or ECMELLA between 2005 and 2019, were retrospectively enrolled from 16 centres in 4 countries. CS was defined at the discretion of the local investigators. Only patients with CS after cardiotomy and minors were excluded. The study was conducted in accordance with the Declaration of Helsinki and was approved by local ethics committees. The primary end point was neurological outcome as a surrogate parameter of quality-of-life, measured by the ‘cerebral performance categories” (CPC) score. Favourable neurological outcome was defined as CPC 1 or 2. The secondary end point was 30-day survival. Predictors for the respective end points were assessed using logistic regression models.
Our results highlight that predictors for 30-day survival are in line with predictors for good neurological outcome. In particular, older age (OR per SD: 30-day survival 0.55, CPC 1-2 0.79), late ROSC (0.76, 0.69) or eCPR (0.58, 0.56) and higher lactate (0.6, 0.49) are associated with similar dismal outcomes as well as hypoxic brain damage (0.55, 0.7).
Conclusion: Predictors of 30-day survival also predict good neurological outcome in CS. Since a survival benefit for ECMELLA has been shown our data implicate that LV unloading with ECMELLA should be considered more frequently in patients with CS. Matching chances of good neurological outcome in ECMELLA patients against VA-ECMO only patients will be investigated next and will be part of the final publication.
|
https://dgk.org/kongress_programme/jt2022/aP1194.html
|