Purpose:
First studies in photon-counting detector-CT prototypes have shown benefits of using ultra
high-resolution coronary computed tomography angiography (UHR-CCTA) over standard
resolution for stenosis detection. However, its use in clinical routine for risk stratification has
not yet been thoroughly investigated. The aim of the present study was to compare UHR-
CCTA on stenosis grading with standard resolution imaging in a clinical cohort with stable
chest pain.
Methods:
Retrospective analysis including all consecutive patients who had undergone UHR-CCTA for
the assessment of coronary artery disease (CAD) with an Agatston Score >0 at the University
Medical Center Mainz since 07/2022. Images were subsequently reconstructed with a slice
thickness of 0.6, 0.4 and UHR 0.2 mm. Stenoses were assessed based on the CAD - Reporting
and Data System (CAD-RADS 2.0). Classification differences between reconstructions were
evaluated using the related samples Friedman’s two-way analysis of variance by ranks. Post
hoc analysis was performed with Wilcoxon signed-rank tests.
Results:
The cohort included 114 patients (37% female; mean age 68±10 years; mean BMI 27±5
kg/m2; mean heart rate 65±10 bpm). Median Agatston score was 242 (range 71-786). CT
identified 190 stenoses with 25% non-calcified, 45% calcified and 30% mixed plaque
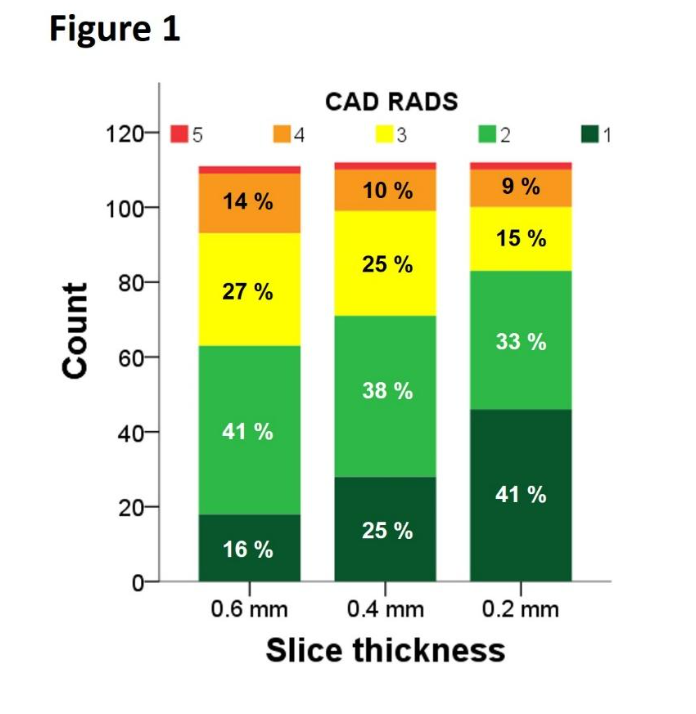
composition. Median per-patient CAD-RADS score was 2 (2-3). With decreasing slice
thickness, the degree of stenosis declined leading to a significant per-patient reclassification
to a lower CAD-RADS category (Figure 1, p<0.001). Compared to the standard 0.6 mm
reconstruction, UHR 0.2 mm reclassified 61% of patients in a lower CAD-RADS category, 31%
in the same category and 8% in a higher category. In the latter patients, the stenoses were
predominantly of non-calcified plaque composition.
Conclusions:
The increased spatial resolution of PCD-CCTA leads to clinically relevant CAD-
Conclusions:
The increased spatial resolution of PCD-CCTA leads to clinically relevant CAD-
RADS reclassification rates in stable chest pain patients. Larger trials are necessary to further
investigate plaque characteristics influencing UHR-CCTA stenosis grading.
https://dgk.org/kongress_programme/ht2023/aV84.html