Introduction
Fixed-dose combination therapies allow combining medications with complementary mechanisms of action and synergistic effects while reducing the patient’s pill burden. The need for combination therapies in hypercholesterolaemia management and in lowering LDL-C has been demonstrated by several trials.1,2 The aim of the SYROS study was to identify key factors driving treatment decision for bempedoic acid 180 mg/ezetimibe 10 mg fixed dose combination (FDC) in the ambulatory setting in Germany.
Study design
SYROS (NCT05546398) combined a physician survey with a retrospective patient chart review in patients with hypercholesterolaemia or mixed dyslipidaemia at high or very high cardiovascular (CV) risk and treated with FDC for ≥4 weeks according to German label.3 Objectives of the survey were to describe the relevance of key factors influencing treatment decisions for FDC, LDL-C treatment goals and LDL-C levels at therapy decision. Main objective of the patient chart review was to characterise patients prescribed with FDC.
Results
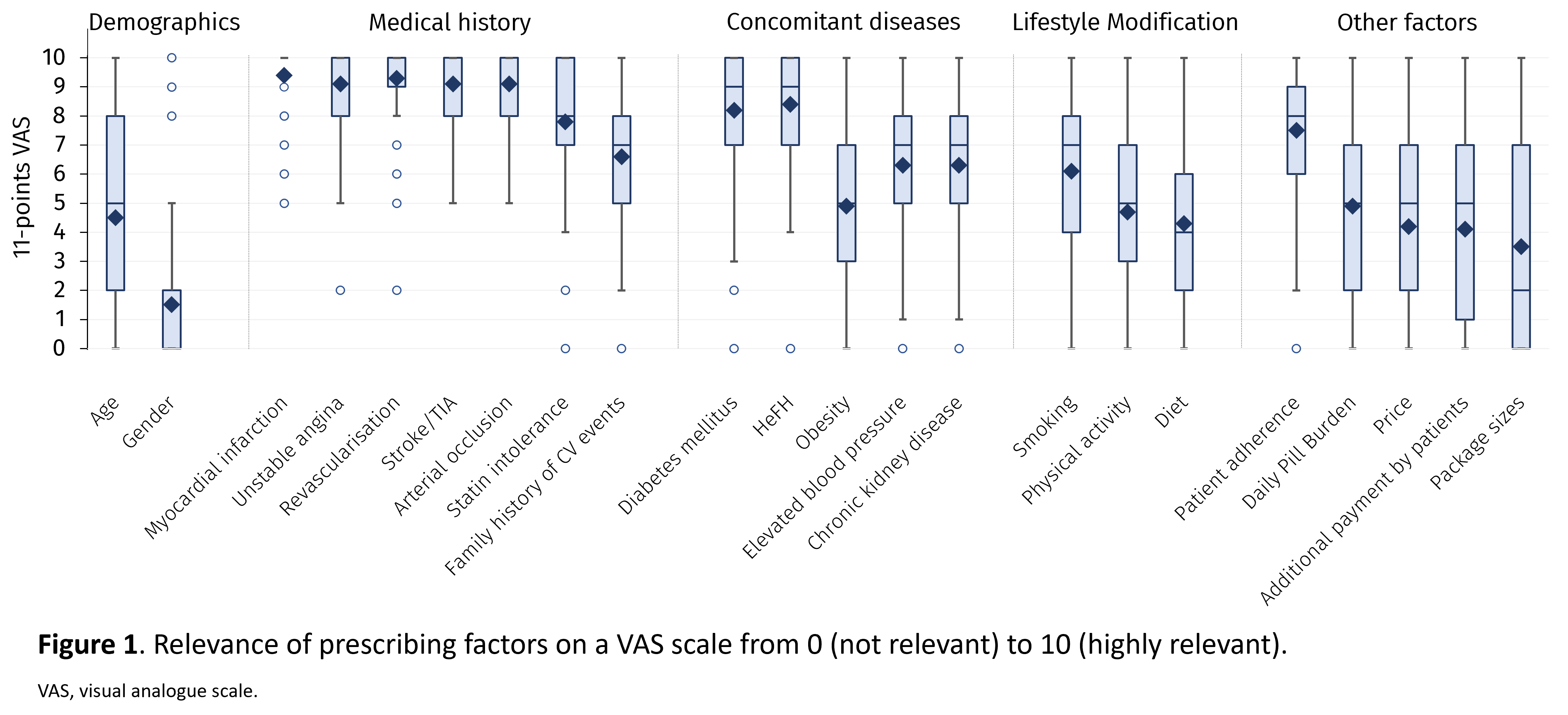
55 office-based physicians provided data on their decision for initiating FDC treatment in a questionnaire. 90.2% stated an absolute LDL-C treatment goal of <70 mg/dL for patients at high CV risk and of <55 mg/dL for patients at very high CV risk, as recommended by current guidelines. Regarding average LDL-C levels considered as threshold for initiation of FDC in patients at high CV risk, 41.8% and 36.4% of respondents stated LDL-C levels >100 mg/dL and >70 mg/dL, respectively. For patients at very high CV risk, 38.2% of respondents indicated LDL-C levels of >70 mg/dL, and 25.5% stated >55 mg/dL as threshold. Most relevant factors for treatment choices were the patient’s medical history, followed by concomitant diseases. Factors like price, package size or additional costs for patients were rated less relevant (Figure 1).
55 office-based physicians provided data on their decision for initiating FDC treatment in a questionnaire. 90.2% stated an absolute LDL-C treatment goal of <70 mg/dL for patients at high CV risk and of <55 mg/dL for patients at very high CV risk, as recommended by current guidelines. Regarding average LDL-C levels considered as threshold for initiation of FDC in patients at high CV risk, 41.8% and 36.4% of respondents stated LDL-C levels >100 mg/dL and >70 mg/dL, respectively. For patients at very high CV risk, 38.2% of respondents indicated LDL-C levels of >70 mg/dL, and 25.5% stated >55 mg/dL as threshold. Most relevant factors for treatment choices were the patient’s medical history, followed by concomitant diseases. Factors like price, package size or additional costs for patients were rated less relevant (Figure 1).
In the retrospective patient chart review of 500 patients, the most common events from medical history were revascularisation (63.2%), myocardial infarction (43.6%), and unstable angina (23.4%). 40.2% of patients were documented as statin intolerant. On average, the last LDL-C measurement prior to treatment with FDC ± statin was 108.8 ± 47.9 mg/dL. At initiation of FDC, 61.0% of patients received concomitant lipid-lowering therapy (LLT) with statins, 6.2% received a PCSK9 inhibitor, and 18.8% any other LLT.
Conclusion
Although the majority of the physicians made their treatment decisions based on current guidelines, there was a high discrepancy between LDL-C treatment goals and LDL-C levels achieved. High LDL-C levels at treatment initiation of FDC and more than 60% of patients receiving FDC as an add-on to statins highlight the need for combination therapy to achieve the LDL-C levels recommended by guidelines. The results from the SYROS study demonstrate that physicians see the FDC as viable treatment option to increase LDL-C goal attainment and improve the management of hypercholesterolaemia.
Although the majority of the physicians made their treatment decisions based on current guidelines, there was a high discrepancy between LDL-C treatment goals and LDL-C levels achieved. High LDL-C levels at treatment initiation of FDC and more than 60% of patients receiving FDC as an add-on to statins highlight the need for combination therapy to achieve the LDL-C levels recommended by guidelines. The results from the SYROS study demonstrate that physicians see the FDC as viable treatment option to increase LDL-C goal attainment and improve the management of hypercholesterolaemia.
Sponsorship
This study was sponsored by Daiichi Sankyo Deutschland GmbH.
1. Ray KK et al. Eur J Prev Cardiol 2021 Sep 20;28(11):1279-1289.
2. Ray KK et al. Lancet Reg Health Eur 2023 Apr 5;29:100624. doi:10.1016/j.lanepe.2023.100624.
3. Nustendi® Fachinformation (last updated: October 2021).
https://dgk.org/kongress_programme/ht2023/aV378.html