Background: A novel catheter combining tip-tissue pressure (contact force, CF) and local impedance (LI) measurement has been recently introduced aiming for enhanced real-time evaluation of catheter stability and lesion formation. However, the influence of CF assessment beyond LI on atrial arrhythmia recurrence has not been elucidated so far.
Objective: To investigate midterm outcome after AT ablation using combined CF and LI assessment compared to LI assessment alone.
Methods: Consecutive patients presenting for AT catheter ablation after previous failed AT or atrial fibrillation ablation were prospectively enrolled. Following initial basket catheter-guided ultra-high-density mapping, ablation was performed using an open-irrigated single-tip catheter (IntellaNav StablePoint, Boston Scientific, Marlborough, MA, USA) capable of continuously assessing CF and LI (CF+LI group). For comparison of mid-term arrhythmia recurrence within the first year after ablation, a retrospective control cohort was analyzed. Here, patients undergoing AT ablation after a previous ablation using the MiFi OI ablation catheter (Boston Scientific) capable of assessing LI only were included (LI group).
Results:
A total of n=22 patients (mean age 71±8 years, 59 % female) were included in the CF+LI group presenting n=30 ATs (left atrial 83 %, makro-reentry 83%, known heart failure 50 %). The LI only control group consisted of n=66 patients (mean age 67±13 years, 48 % female, heart failure 38 %, n=95 ATs). Baseline patient characteristics were similar between groups. Table 1 displays procedural characteristics. The median procedure duration was longer (p=0.01) and fluoroscopy time shorter in the CF+LI group (p=0.004). Most common critical AT isthmus localizations were observed at the left atrial anterior wall (CF+LI 28 % vs LI 18 %, p=0.004) and roof (17 % vs 19 %, p=0.41). Total ablation time (p=0.25) did not differ between groups. A total of n=948 were analyzed in the CF+LI group. The maximum LI drop (∆LI) during RF delivery was strongly related to baseline LI (r=0.73, p<0.001), while only minorily to the mean CF (r=0.13, p<0.001) and minimum CF (r=0.15, p<0.001) during ablation.
The median follow-up duration was longer in the LI vs CF+LI group (304 vs 190 days, p<0.001). Recurrence of any atrial arrhythmia within the first year after ablation beyond a blanking period of 3 months was similar between both groups (Figure 1).
Conclusion:
Combination of LI and CF allows for real-time assessment of catheter stability and lesion formation. However, mid-term outcome was similar compared with LI assessment alone and remains challenging in patients undergoing re-do AT ablation. Further studies are needed to optimize ablation strategies using combined CF and LI assessment.
Table 1. Procedural characteristics
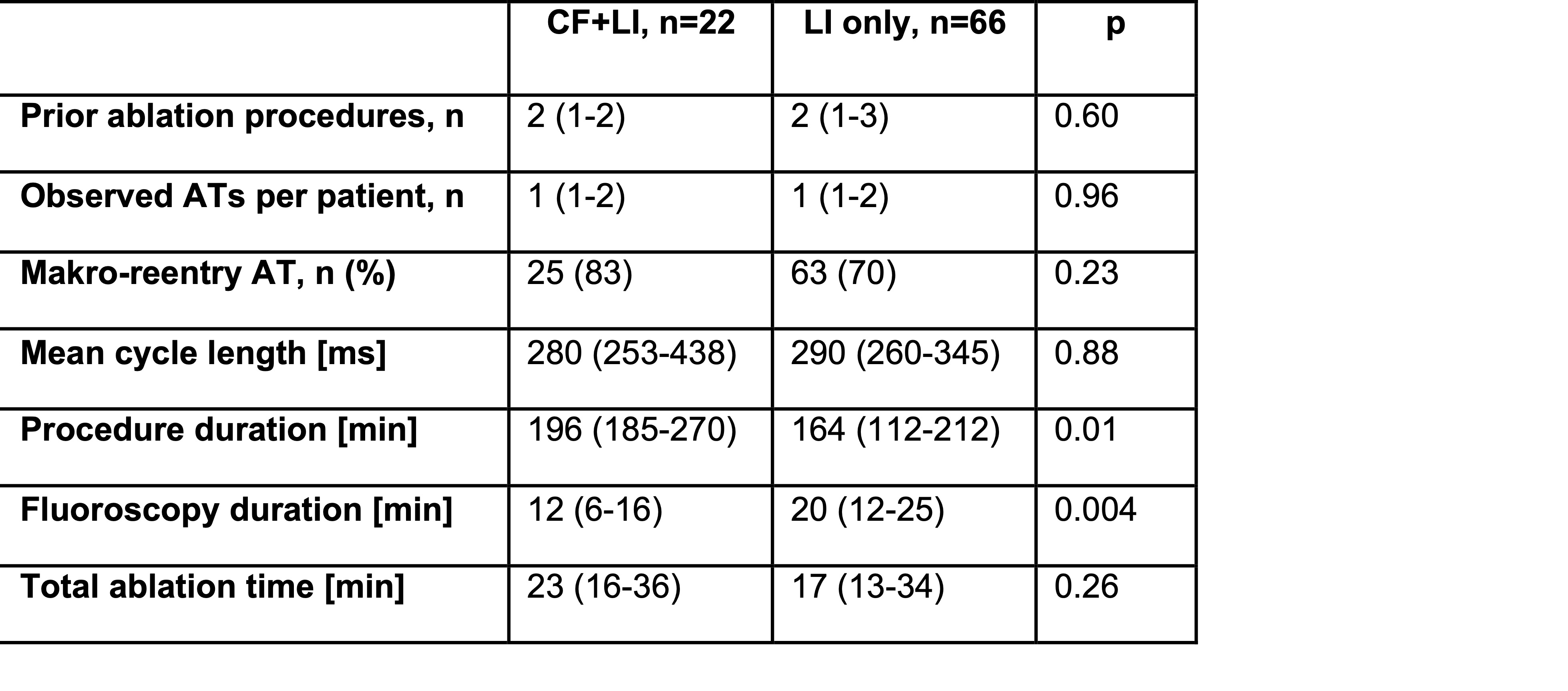
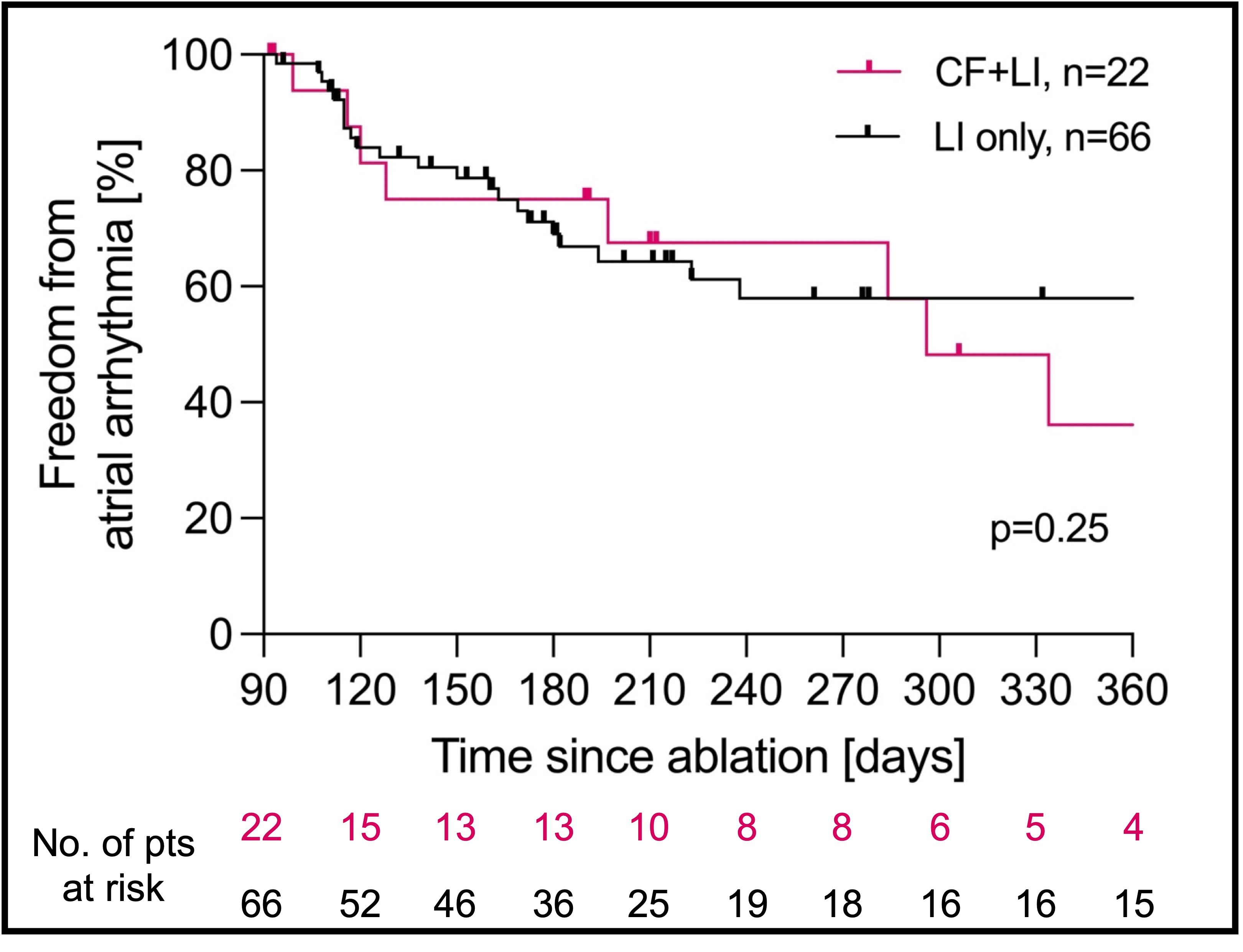
Figure 1. Follow-up during the first year after AT ablation using combined CF and LI vs LI assessment only.
https://dgk.org/kongress_programme/ht2022/aP302.html