Clin Res Cardiol 108, Suppl 2, October 2019
|
|
A case report: Idiopathic Right Ventricular Outflow Extrasystolie - Not as benign as we think ?
|
|
M. Scholten1, H. Bogossian1, A. Khan1, Z. Karosiene2, Q. S. Nguyen2, B. Lemke2, M. Zarse2
|
|
1Innere Medizin III / Kardiologie und Angiologie, Märkische Kliniken GmbH, Lüdenscheid; 2Märkische Kliniken GmbH, Lüdenscheid;
|
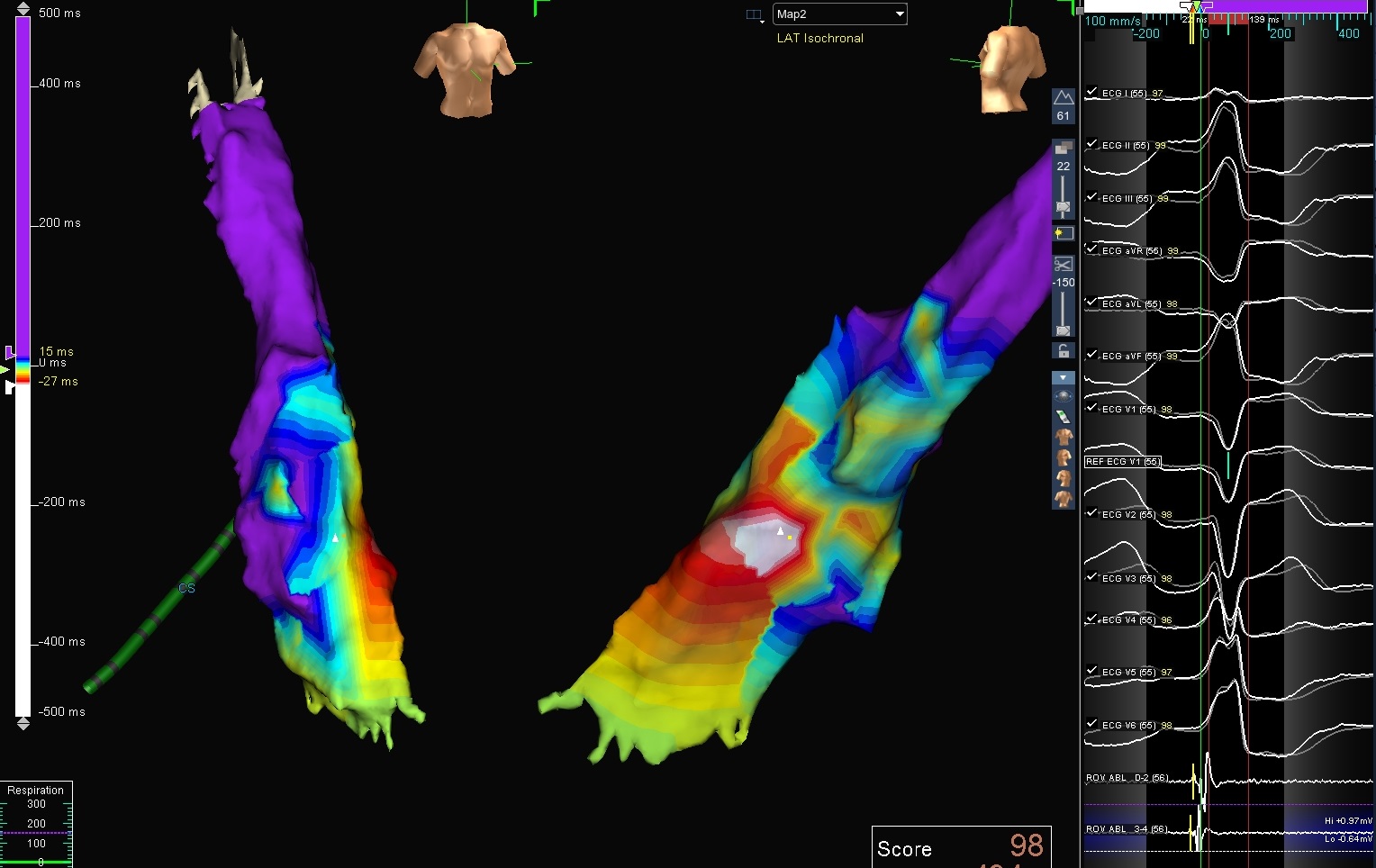
An 80y old male patient presented himself in the emergency department (12/2018) suffering from palpitations resulting in lightheadedness, dizziness and presyncopes within the last 24 hours. In 2012 he underwent a successful RF-ablation of idiopathic VPCs stemming from the left ventricular outflow tract (LVOT). Additionally he suffered from episodes of paroxysmal atrial fibrillation (AF). The patient had a normal blood test and showed arterial hypertension and hypercholesteremia as sole cardiac risk factors. The echocardiography demonstrated a reduced EF of 50% with a diastolic relaxation disorder. Angiography ruled out cardiac artery disease (CAD) (08/2018). The surface ECG demonstrated VPCs with an inferior axis and a left bundle branch block deformity of the QRS complexes with R/S transition in V3/V4 corresponding to an origin of the idiopathic VPCs is the lateral right ventricular outflow tract . The underlying sinus rhythm showed normal PQ (180ms), QRS (110 ms) and normal repolarization time (410 ms). An electrophysiological examination with electroanatomical mapping (NAVX, St. Jude edical,Minneapolis, USA) was performed. Local activation mapping identified the spot of earliest activation at the posterolateral RVOT (Figure 1), 24 ms before QRS onset .
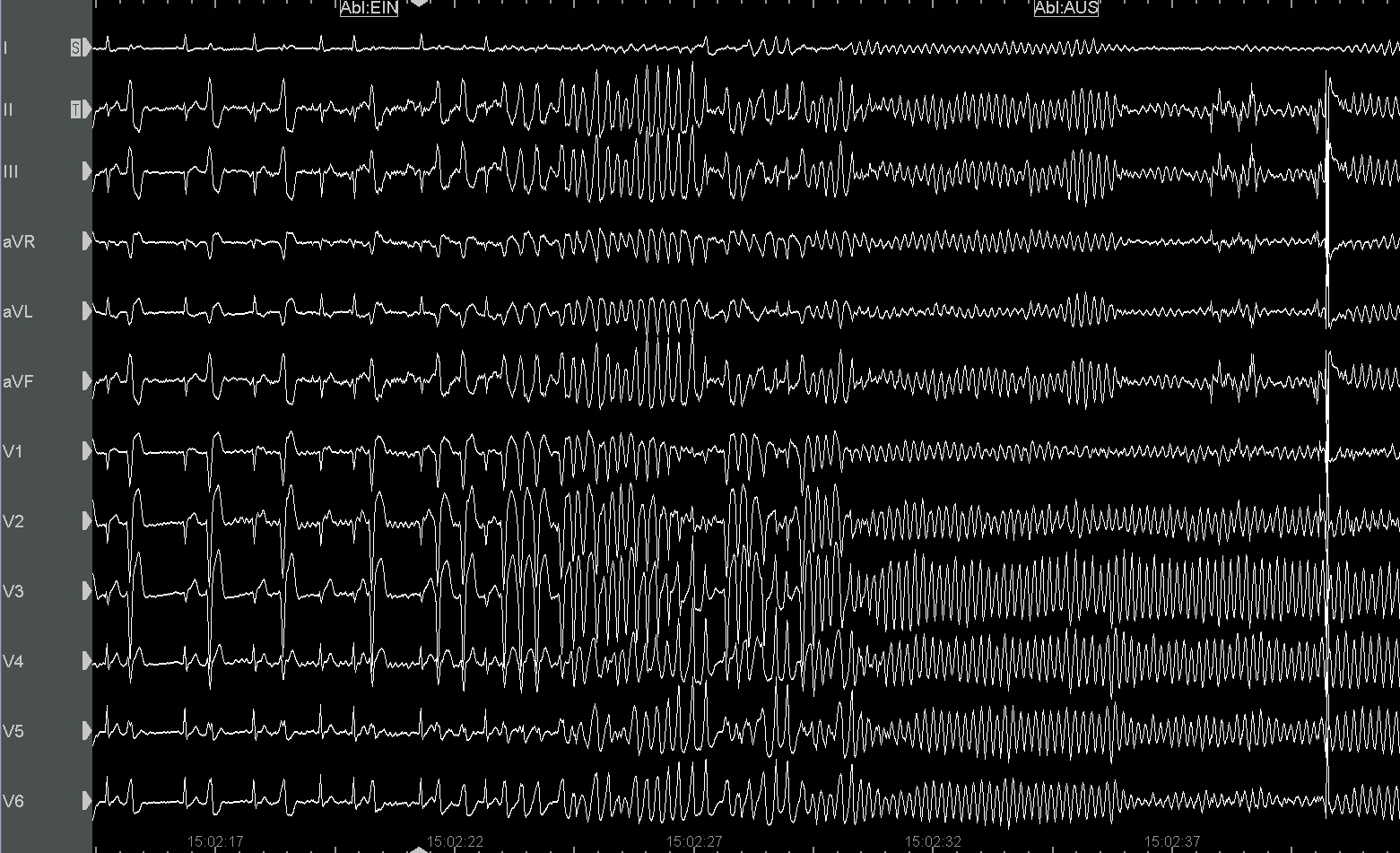
Radiofrequence ablation at this spot of earliest activation initially evoked increasing VPCs rapidly transforming into a fast VT. We intitially welcomed the VPCs as proof to have effectively targeted the precise spot of abnormal excitation. Whereas a VT, evoked by ablation would generally subside within a few seconds after ablation was terminated, this ever accelerating RVOT, displaying a torsade de pointes like appearance continued even in the absence of further ablation heat, thus being hemodynamically dramatically detrimental (Figure 2).
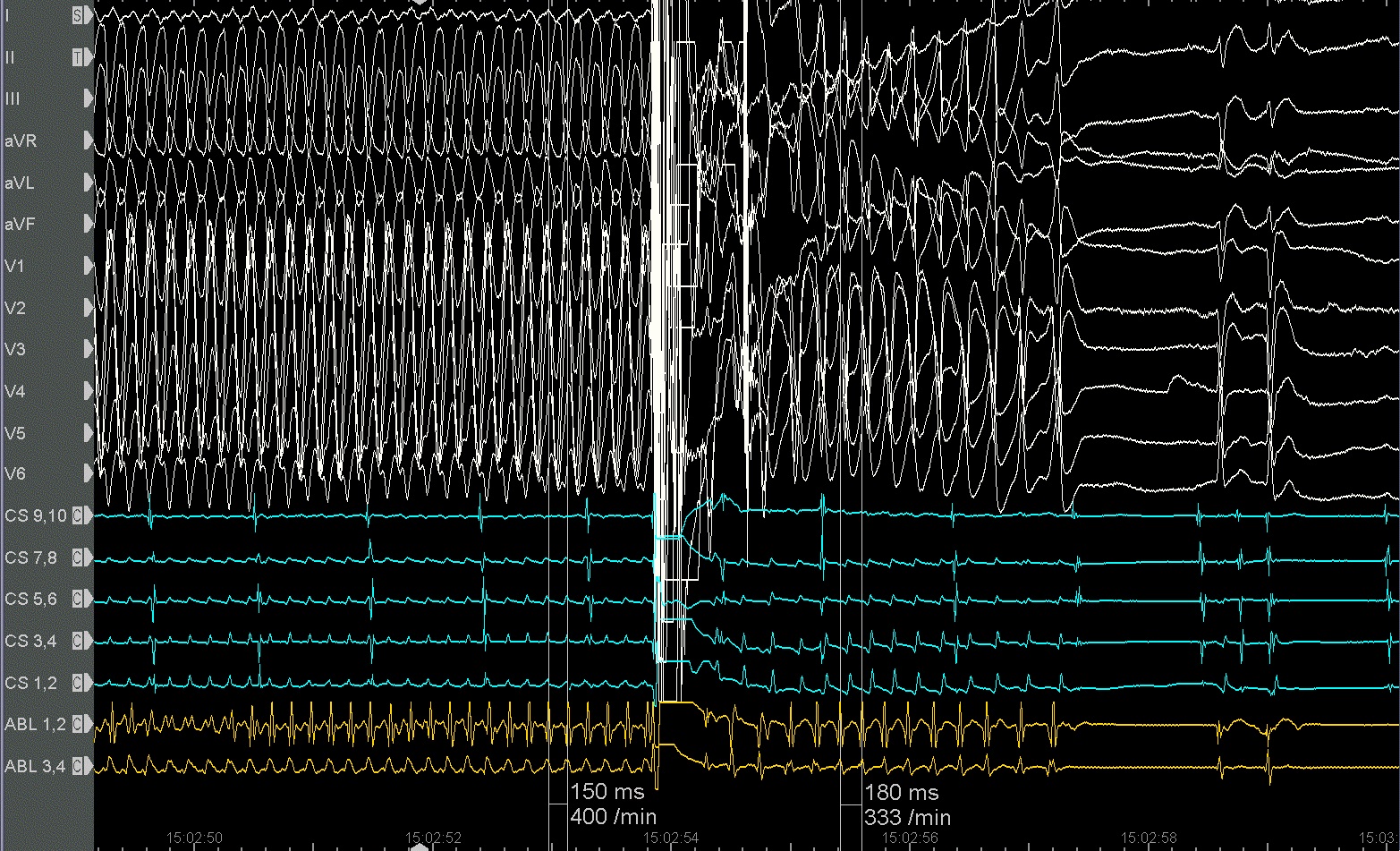
According to to ERC guidelines we defibrillated the patient which slowed down the tachycardia from 400bpm (CL 150ms) to 333bpm (CL 180ms), demasking our intial RVOT which then terminated within 4 seconds (Figure 3). After defibrillation the heart rhythm was stable again and ablation was continued without any more triggering of VPCs. After ablation was finished, neither programmed electrical stimulation nor injection of Orciprenaline (Alupent® 0.1mg) could induce any more form of VPC (Figure 6). The routine postprocedural monitoring for 24h was completely uneventful.We present the rare case of a RVOT ablation triggering a fast hemodynamically unstable tachycardia requiring defibrillation to prevent cardiac arrest. We can only speculate whether an alternative intrinsic trigger such as sympathicoadrenergic stimulation might also had the potential to induce this potentially fatal VT.
|
https://www.abstractserver.com/dgk2019/ht/abstracts//P687.htm
|